Effects of Fasting in Ramadan on Pregnancy Outcome: Systematic Review
- Corresponding Author:
- Mehreen Jamshed
Department of Pharmacy, Jinnah University for Women, 5C, Nazimabad, Karachi, Sindh, Pakistan
E-mail: mehreensalman125@gmail.com
Received: 27-Apr-2021, Manuscript No. ijocs-22-61934; Editor assigned: 29-Apr-2021, PreQC No. ijocs-22-61934(PQ); Reviewed: 09-May-2022, QC No. ijocs-22-61934(QC); Revised: 14-May-2022, Manuscript No. ijocs-22-61934(R); Published: 30-May-2022, DOI: 10.37532/1753-0431.2022.16(4).242
Abstract
Methods: Complying with Prisma guidelines, a cross-sectional study was conducted based on an Electronic database searched across PubMed, Web of Science, Cochrane, and Scopus, without date restrictions. Our inclusion criteria were pregnant women in any one trimester during the 30 days of Ramadan. Four groups were made for the sample: non-fasting, fasting in first 10 days, fasting in 2nd trimester, and fasting in the last 10 days. Meta-analysis was conducted in random-effects using Covariance analysis and the SPSS programme for screening of relevant data.
Results: A total of 43 articles were included after screening and the data for various pregnancy outcomes were measured. Fetal biparietal diameter (BPD) was found to be increased by 0.2mm in all trimesters. The data proved no significant difference in BMI with mother's age, start of pregnancy, multi gravida or history of abortion. For the effects on neonatal health, no significant correlation was found between the number of days they had fasted and neonate’s height, weight, or head circumference. No statistically significant relationship between fasting during different trimesters and pregnancy outcome indicators.
Conclusion: Fasting had no adverse effects on pregnant women or fetal growth. Further study, if possible, a randomized controlled study, is needed to determine whether maternal fasting did not affect maternal-fetal health.
Keywords
Pregnancy; Maternal health; Ramadan fasting; Fetal health
Introduction
Along with pilgrimage, prayer, charity, and faith, Islam’s five pillars include Ramadan. During Ramadan all healthy persons should fast from sunrise to nightfall. The Quran, on the other hand, exempts pregnant and nursing women from fasting if it might jeopardize their health and that of their unborn children [1]. Many pregnant and nursing women fast throughout Ramadan for Causes of social, cultural and religious significance [2,3]. Ramadan s observed according to It takes 29 days to 30 days since it begins 11 days or 12 days sooner than the previous year. In effect, this implies that nearly three-quarters of Muslim women’s children will be required to fast during Ramadan [4]. The effects of Ramadan fasting on mother and child health are unknown. Several studies on this topic have often produced conflicting results [5]. For example, it is believed that fasting during Ramadan affects the biophysical properties of the fetus and the respiratory system [6]. Another repeating theme in the research was the effect of Ramadan fasting on the health of women who were already afflicted with diabetes or cancer [7-10]. Fasting during Ramadan, on the other hand, has been shown to be harmful to healthy pregnant women and their children. Moreover, several researches on the effects of fasting during Ramadan have been conducted. They did not, however, offer a thorough assessment of the current investigation, focusing instead on shortterm perinatal outcomes without taking longterm implications into account [11-13]. Effective communication of alternatives and guidance is often missing since pregnant and nursing women, as well as healthcare professionals who desire to fast, are often uninformed of the ramifications of fasting during Ramadan. Women, for example, are typically afraid of being rejected if they notify their doctors about their fasting plans [14]. Given that most Muslim women also experience Ramadan in the womb, it’s worth considering whether a solution can be found. The purpose of this study was to collect all available information about Ramadan fasting and the health implications of pregnancy for offspring.
Methods
On the advice of, a cross-sectional investigation was carried out. Electronic database searched across PubMed, Web of Science, Cochrane and Scopus. No date restrictions were present for the literature search. Each database required several search terms related to “fasting”, “Ramadan”, and “pregnanacy” and these were evaluated for “fetal growth indices”, “birth indices”, “cognitive effects” and “long-term effects”
■ Study selection
The articles we analyzed for our study were screened by their abstract. Only those articles which followed our inclusion criteria were included.
■ Inclusion criteria
Articles that proved searches on offspring developmental parameters and health. The offspring developmental parameters included were birth indices, growth indices, long-term effects and cognitive effects. Articles with full text were examined and included.
■ Exclusion criteria
• Animals other than humans have been used in studies
• Studies based on women who had a health problem that wasn’t related to pregnancy
• Systematic and narrative review
• Other than English, studies are written in other languages
• Exposure to only one day of Ramadan
• Studies based on other traditions of Islam other than Ramadan
■ Data extraction
After selecting all studies and reviewing their inclusion and exclusion criteria. We determined the demographics and sample size for each study, as well as study location, testing procedures, impacts, and outcomes.
The following performance indicators were collected
• Indexes of fetal growth, “estimated fetal birth weight, Biparietal Diameter (BPD), Femurlength (FL), fetal weight gain, abdominal circumference, Amniotic Fluid Index (AFI), biophysical profile (breathing movements, gross body movements, etc.), biophysical score, Non-Stress Test (NST) and Doppler indices”
• Indicators of birth; “birth weight, birth length, Birth Head Circumference (HC), Pretermdelivery (PTD), gestational length, Low Birth Weight (LBW), mode of delivery, fetal Apgar score, congenital anomalies, perinatal mortality”
• Effects on the mind: “test scores, mental/ learning disabilities, IQ scores”
• “BMI (Weight and Height), disease or condition (diabetes, anemia, cardiovascular symptoms, shortness of breath), general health throughout life, mortality before 5 years” are some of the long-term effects.
■ Quality assessment
Carter et al. provided a technique, while the National Collaborating Center for Methods and Instrument suggested a standard [15,16]. Use this method to evaluate the quality of your articles. These tools have been adapted for research based on their (ethical) feasibility. In five categories, each article received a score of zero, one, or two: research design, study size, exposure, and impact. conclusions results, and alterations. Each article received low (5) scores, medium (5-7) scores, and high (>7) scores. Part of the results was a detailed paper “A Study on the Impact of Medium and High-Quality Ramadan on Children’s Health”.
Results
■ Study selection
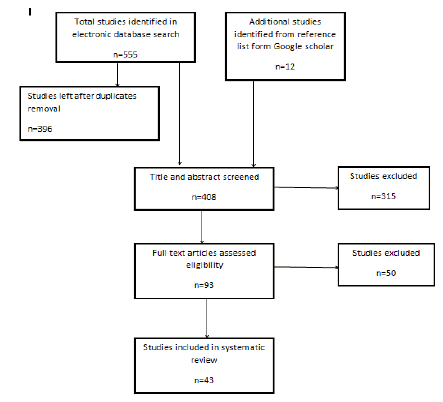
On Figure 1 is a PRISMA flowchart for the analysis of articles in systematic reviews. An electronic search of the database yielded a total of 555 entries. There were 396 studies left after duplicates were deleted. A total of 12 new papers were added, all of which were found Via PubMed and Medline. Three hundred and fifteen papers were eliminated After evaluation of the full text, 50 others were rejected due to title and abstract.
Study characteristics
We have tabulated and organized our research article (n=43) according to the outcomes defined. Fetal growth indices outcomes were defined by nine articles. Birth indices was focused by nine articles. cognitive effects were explored by four articles. Prenatal exposure in Ramadan; long-term effects were found by eight articles. There were observational studies included in our research from which cross-sectional were five. We utilized 6 case-control studies and 21 retrospective cohort studies (half of which were prospective). A total of 11 prospective cohort studies were analyzed. The mean study quality score was 5.4 on a scale of 2 to 9.
■ Fetal Growth Indices (FGI)
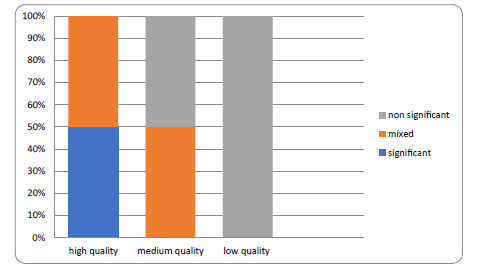
The outcome of fasting in Ramadan on pregnant women and fetal growth has been shown in Figure 2. There is only one quality document from the FGI comparing a group of Fasting and fasting women. No difference in Non-Exercise Test (NST) sensitivity, biophysical characteristics, or Umbilical and Arterial Doppler Index (MCA) and Amniotic Fluid Index (AFI) was found in this article ) (p>0.05). When we compared the medium-quality studies, a total of four, no fetal growth indices were affected by fasting [17-21]. In three studies, Women In the second or third trimester, women who fasted had lower AIF levels than women who were fasting [21-23]. However, fetal Biparietal Diameter (BPD) was found to be increased by 0.2 mm in Karateke et al. [22] study in all trimesters. Further, in a study by Sakara et al. They significantly affected head circumference, femur length, and BPD (p<0.05) [23].
Birth indices
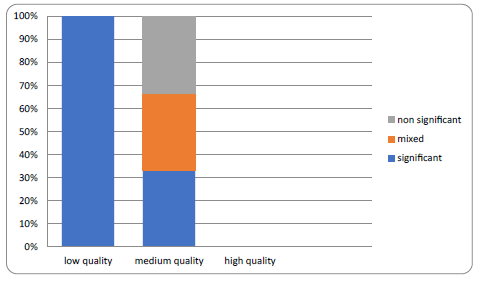
The outcome of birth indices has been shown in Figure 3 of fasting pregnant women. Different groups were compared i.e. Uncontrolled for three months, fasting and fasting every three months, fasting and fasting, fasting and fasting days, and uncontrolled for three months. The comparison of groups is separately discussed for accuracy.
In a high-quality study comparing fasting and non-fasting mothers, the mean birth weight of exposed offspring was found to be significantly lower (p=0.024, 108 g) [24]. Although Kavehmanesh and Abolghasemi found an increase in birth weight per 100 g in the multiple regression models including BMI, the difference between fasted and non-fasted groups disappeared (p=0.009) [25]. age and education In other words, the confusing situation explains the obvious meaning. However, there were no significant variations in birth weight between those who fasted and those who did not fast. women according to 13 questionnaires of medium and high quality [19,21,22,26-35]. In Birmingham, Cross et al. studied Moms and children of Asian Muslim women, white and non-Muslim mothers. [36]. Between the three groups, there were no significant variations in birth weight. Five studies showed no change in % LBW between fasted and non-fasted groups [22,28,29,31,32]. Moreover, half of the studies comparing fasting and fasting Preterm Birth in women is rare (PR) in either group [19,24,25,28,31,32]. Two studies of moderate quality compared maternal birth weights with controls [34,37]. After analyzing various key characteristics such as Socioeconomic Status (SES) and smoking, infants are at risk of low birth weight during Ramadan (272.1, p=0.05) [37]. The study found that Control and fasting groups showed no signs of weight loss within three months after assessing a similar set of confounders four years later [34]. In the absence of a control group, During Ramadan, two studies [38,39] looked at the birth weight of fasting women with various pregnancies. There were no variations in gestational age, delivery time, or HC between fasting and non-fasted pregnancies, according to Ziaee et al. [39]. Birth weight was highest in the first trimester and lowest in the second trimester (3411 g, p=0.03), according to Salafraz et al. [38]. In three months, however, the frequency of LBW did not alter much. Four studies [32,36,37,40] examined changes in fasting days and fertile days. Three of these studies included a fasted control group and three control groups (1 day-10 days of fasting; 11 days-20 days;>20 days) [32,36,38]. Savery et al. studied the children of women who fasted for two to almost two weeks for no apparent reason [37]. In none of these studies was there a statistically significant association between fasting days and reproductive performance. (eg. low birth weight, birth type, head length or circumference). The method of delivery was studied in five questionnaires [19,24,27,32,41]. Three of these studies included a fasted control group and three control groups (1 days-10 days of fasting; 11 days-20 days; >20 days) [32,36,38]. safe and colleagues [37] compared the children of mothers who fasted for two weeks for no reason. There was no statistically significant link between fasting days and weight reduction in these trials. (Low) birth weight, birth type, head length or circumference are examples of fertility measurements. Five surveys [19,24,27,32,41] looked into the delivery technique.
■ Effects on the mind
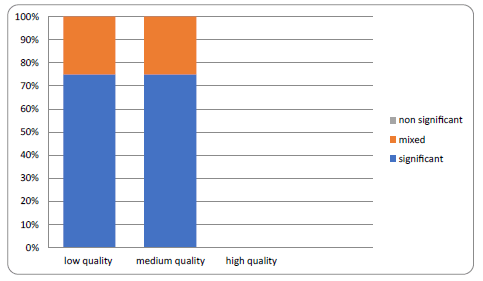
The amount of evidence for Figure 4 depicts the impact of Ramadan on offspring cognition. Three studies of moderate quality looked at the impact of Ramadan on cognition [42-44]. Aziz et al. observed no significant difference in IQ scores between the treatment and control groups in children aged 4 to 13 [43]. The effect size according to Majid and Almonda et al. was 7.4% [50]. Other studies showed significant effects in the first trimester of pregnancy reduction in cognitive test scores and an 8.4% reduction in math test scores (p=0.01 for both) [38,42]. This is the result of reading, writing, and math with a standard deviation of 0.05-0.08. Nutrients Review 2021 7, 13 of 14 4. Fasting during Ramadan and cognitive impairment during pregnancy.
■ Long-term consequences
The long-term consequences of fasting during Ramadan were investigated in four studies of intermediate quality (Figure 5) [45-48].
Muslims who survived Ramadan before birth had worse overall health (SD 6.1%, p=0.01), blood pressure, haemoglobin levels, and lung capacity, according to Van Ewijk [47]. This effect was stronger in people over 45 (18.5%, p=0.01) and in the second trimester at the start of Ramadan. Albazar and colleagues discovered this in the second trimester. [45] found that the duration and length of pregnancy of boys and girls born to mothers affected by Ramadan differed significantly from their peers (p=0.005 and p=0.04). According to the same Indonesian Family Life Study (0.93 kg, 95% confidence interval), Muslims had a lower BMI in the second and third months of Ramadan due to weight loss 1.72, 0.14 and 1.06 kg (95% CI), (-1.88, 0.25) higher than in unborn children during Ramadan [48]. Albazar and his colleagues discovered it in the second trimester. [45] found that the duration and length of pregnancy of boys and girls born to mothers affected by Ramadan differed significantly from their peers (p=0.005 and p=0.04). According to the same Indonesian Family Life Study (0.93 kg, 95% confidence interval), Muslims had a lower BMI in the second and third months of Ramadan due to weight loss. 1.72, 0.14 and 1.06 kg (95% CI), (-1.88, 0.25) higher than in unborn children during Ramadan [48] (Table 1).
Table 1: list of studies categorized on the basis of outcome.
| Outcome | Sources |
|---|---|
| Birth indices | Almond and Mazumder, 2011 [4], Hizli et al., 2012 [19], Seckin et al., 2014 [21], Karateke et al., 2015 [22], Awwad et al., 2012 [24], Kavehmanesh and Abolghasemi, 2004 [25], Rezk et al., 2016 [26], Altunkeser and Körez, 2016 [27], Daleyet al., 2017 [28], Makvandi et al., 2013 [29], Ozturk et al., 2011 [30], Petherick et al., 2014 [31], Safari et al., 2019 [32], Sarafraz et al., 2014 [33], Savitri et al., 2018 [34], Shahgheibi et al., 2005 [35], Cross et al., 1990 [36], Savitri et al., 2014 [37], Sarafraz et al., 2015 [38], Ziaee et al., 2010 [39], Sakar et al., 2016 [40], Jamilian et al., 2015 [41], Alwasel et al., 2010 [49], Arab andNasrollahi, 2001 [50], Boskabadi et al., 2014 [51], Savitri et al., 2019 [52], Tith et al., 2019 [53] |
| Fetal growth indices | BayogluTekin et al., 2018 [17], Dikensoy et al., 2008 [18], Hizli et al., 2012 [19], Moradi, 2011 [20], Seckin et al., 2014 [21], Karateke et al., 2015 [22], Sakar et al., 2015 [23], Rezk et al., 2016 [26], Mirghani et al., 2003 [54] |
| Long term effects | Alwasel et al., 2011 [45], Mandemakers, 2018 [46], Van Ewijk, 2011 [47], Van Ewijket al., 2013 [48], Alwasel et al., 2013 [55], Karimi and Basu, 2018 [56], Kunto and Pradella and van Ewijk, 2018 [57], Schoeps et al., 2018 [58] |
| Cognitive effects | Almond and Mazumder 2011 [4], Almond et al., 2014 [42], Azizi 2004 [43], Majid 2015 [44] |
Discussion
In various studies, fasting during Ramadan has been associated with fetal growth rate, birth rate, cognition, and long-term outcomes. On the other hand, important conclusions are drawn mainly from poor quality surveys. There was no significant effect on fetal development, childbirth, cognitive performance, or qualitative long-term outcomes. While most moderatequality studies showed mixed or negligible results for long-term effects, most moderate-quality studies showed significant results for short-term effects. Previous studies have shown that fasting during Ramadan does not negatively affect the health of healthy pregnant women and their children. Although Rouhani and Azadbakht did not find a significant effect, they advise against fasting during Ramadan due to the limitations of the studies included in their analysis. Glaser and colleagues believe that more research is needed to comprehensively explore the relationship between maternal and child health. They found no evidence of an adverse effect of Ramadan on birth weight, but their systematic review and meta-analysis did not find sufficient evidence for a possible effect on later perinatal outcomes. According to Nick et al., fasting Ramadan did not affect the physical and mental development of the embryo. While most studies have not found an association between fasting during Ramadan and fetal measurements, three studies have found a decrease in AIF. When all other fetal symptoms are normal, high fever and prolonged fasting can lead to maternal dehydration. Perinatal mortality, fetal malformations, PTD, NMT, and poor neonatal health are associated with low amniotic fluid levels. Therefore, it is necessary to pay special attention to the pregnancy of these women. Anthropometric measurements at birth are considered predictors of postpartum mortality. Therefore, it is important to determine whether maternal fasting has a significant impact on these performance measures. Overall, no relationship was found between maternal hunger and anthropometric outcomes. In multivariate analyses, where this relationship was attenuated, the differences were very small or were not adjusted for factors that could explain the significant results. One of the first studies to find a link between fasting Ramadan in the womb and a leaner, shorter body later in life was one of the first to show a link between fasting Ramadan in the womb and a leaner, shorter body at a later age. The first study to show an association between fasting in the womb in Ramadan and a leaner and shorter body later in life is one of the first to show a link between fasting in the womb in Ramadan and the thinness Paradigm. Fetal programming is a phenomenon that occurs when the mother’s food affects the fetus.
The ability of the placenta to deliver nutrients is reflected in its mass and surface shape. Thus, the size and shape of the placenta at birth may be associated with chronic disease later in life. During the “Great Leap Forward” in China from 1959-1961, research showed that prenatal fasting resulted in lower BMI later in life. Maternal malnutrition during pregnancy can have serious long-term health consequences for adults, according to the Dutch Antenatal Hunger Study. Fasting in the first trimester is associated with coronary heart disease and obesity, while fasting in the second trimester is associated with increased microalbuminuria and obstructive airway disease. Although total caloric intake did not decrease significantly during Ramadan, the metabolic effects of fasting during pregnancy are expected to be comparable to those of feasting or fasting. In addition, early research suggests that if a mother does not eat or drink for more than 13 hours, it can lead to a stress response. As a result, fasting can put the fetus in danger during Ramadan. Environmental cues suggesting that the outside world outside the uterus will have special properties can trigger epigenetic processes that lead to different gene expression phenotypes. If the intrauterine environment of the fetus and the postpartum environment do not match, the fetus is destined for harsh environments, This may or may not work. For example, prenatal stress hormone exposure can train the hypothalamic-pituitaryadrenal axis (which regulates the endocrine system, including the stress response), leading to later blood pressure spikes and type 2 diabetes. and cardiovascular risk factors were better after exposure. However, given the mediocre quality of the study, the results should be interpreted with caution. Keep in mind that the general “Ramadan effect” rather than the specific “fasting effect” may complicate long-term cognitive, anthropometric, and medical outcomes. For example, iftar (sunset festival) is often eaten with greasy, oily, and sweet foods. Instead of harming the fetus by reducing calories (fasting), iftar can counteract the effects of fasting by consuming energy-rich foods. Ramadan also disrupts normal nighttime sleep, especially for those in charge of food preparation. Of course, when considering the “influences of fasting”, Consideration should be given to the type of food consumed during iftar and sleep habits. The search covers a large number of keyword strings covering a wide range of topics related to Ramadan fasting, pregnancy, and childbearing. The search is also carried out in many databases. However, The quality of the studies included in this review was generally poor, which is a weakness of this study. This loss of control over important confounding variables occurs in the vast majority of experiments and is especially problematic. As a result, there has been much confusion as to whether there is any Bias that can affect results. Another problem is that many studies choose to fast for Ramadan because of the timing. and pregnancy dates (combined with religion, ethnicity, or language). Because data on Ramadan fasting practices are not publicly available, it is not known if and how often or strictly women fast. This possible misclassification may lead to underestimation or exaggeration of the effects of fasting. Also, research studies that have included true fasting as part of determining the impact of Ramadan have come up with mixed results. For example, some studies compare women who fast for an entire month with women who fast or don’t fast at all. Others compared women who fasted for a month with those who fasted moderately or did not fast at all. The associated variability usually makes the full effect is difficult to measure. The long-term cognitive effects of fasting during Ramadan should be the subject of future research, preferably using a prospective research project with a large number of people. Sociological and theological aspects of Ramadan may influence mothers’ behavior, supporting the hypothesis that Ramadan does not affect children, so this prospective study should be undertaken with caution. Another promising way to study these effects is to use a modified retrospective study design based on conventional data collection comparing Islamic pregnant women during Ramadan and Ramadan to reduce confusion, but only when it is prohibited during routine registered care. Effects may still be seen due to birth outcomes such as malaria and vitamin D levels. These tests should also confirm results regarding labor and fetal health. In addition to their normal diet, women should pay close attention to the quality of their meals during Ramadan. The total caloric intake of pregnant women during Ramadan was similar as carbohydrate-rich diet was increased and proteins were reduced. Ramadan fasting with prior patient education and medication adjustment makes modest benefits of fasting on metabolic profile and body composition.
In addition to this quantitative study on the impact of fasting during Ramadan, we support qualitative research on communication between pregnant women and their health care providers to improve decision-making about joint fasting during pregnancy.
Conclusion
Our study findings suggest that fasting had no adverse effects on pregnant women intrauterine growth or birth-time markers. Whereas pregnant women who fasted during their first trimester were found to develop neonate’s low-birthweight risk compared with non-fasting. This reveals the need of special nutrition support for fasting pregnant women.
Data Availability
All data is available online.
Conflict of Interest
All authors declare no conflict of interest.
Funding
None available.
References
- Adawi M, Watad A, Brown S, et al. Ramadan Fasting Exerts Immunomodulatory Effects: Insights from a Systematic Review. Front Immunol 8, 1144 (2017).
- Mirsane SA, Shafagh S. A Narrative Review on Fasting of Pregnant Women in the Holy Month of Ramadan. J Fasting Health 4, 53-56 (2016).
- Kridli SAO. Health Beliefs and Practices of Muslim Women During Ramadan. MCN Am J Matern Nurs 36, 216-221 (2011).
- Almond D, Mazumder B. Health Capital and the Prenatal Environment: The Effect of Ramadan Observance During Pregnancy. Am Econ J Appl Econ 3, 56-85 (2011).
- Mirghani HM, Weerasinghe S, Al Awar S, et al. The Effect of Intermittent Maternal Fasting onComputerized Fetal Heart Tracing. J Perinatol 25, 90-92 (2004).
- Van Bilsen LA. Savitri AI, Amelia D, et al. Predictors of Ramadan fasting duringpregnancy. J Epidemiol Glob Health 6, 267-275 (2016).
- Afandi BO, Hassanein MM, Majd LM, et al. Impact of Ramadan fasting on glucose levels in women withgestational diabetes mellitus treated with diet alone or diet plus metformin: A continuous glucose monitoring study. BMJ Open Diabetes Res Care 5, e000470 (2017).
- Hassanein M, Al Arouj M, Hamdy O, et al. Diabetes and Ramadan: Practical Guidelines. Diabetes Res Clin Pract 126, 303-316 (2017).
- Pathan F. Pregnancy and fasting in women with diabetes mellitus. J Pak Med Assoc,65, S30-S32 (2015).
- Bragazzi NL, Briki W, Khabbache H, et al. Ramadan Fasting and Patients with Cancer: State-of-the-Art and Future Prospects. Front Oncol 6, 27 (2016).
- Rouhani MH, Azadbakht L. Is Ramadan fasting related to health outcomes? A review on the related evidence. J Res Med Sci 19, 987-992 (2014).
- Zoukal S, Hassoune S. The effects of Ramadan fasting during pregnancy on fetal development: A General Review. Tunis Med 97, 1132-1138 (2019).
- Rabinerson D, Dicker D, Kaplan B, et al. Hyperemesi gravidarum during Ramadan. J Psychosom Obstet Gynecol 21, 189-191 (2000).
- Carter P, Gray L, Troughton J, et al. et al. Fruit and vegetable intake and incidence of type 2 diabetes mellitus: Systematic review and meta-analysis. BMJ 341, c4229 (2010).
- National Collaborating Centre for Methods and Tools. Quality Assessment Tool for Quantitative Studies, Hamilton, ON: McMaster University (2017).
- Tekin YB, Guven ESG, Ural UM, et al. Evaluation of the effects of fasting associated dehydrationon maternal NGAL levels and fetal renal artery Doppler parameters. J Matern Neonatal Med 29, 629-632 (2015).
- Dikensoy E, Balat O, Cebesoy B, et al. Effect of fasting during Ramadan on fetal development andmaternalhealth. J Obstet Gynaecol Res 34, 494-498 (2008).
- Hızlı D, Yılmaz SS, Onaran Y, et al. Impact of maternal fasting during Ramadanon fetal Doppler parameters, maternal lipid levels and neonatal outcomes. J Matern Neonatal Med 25, 975-977 (2011).
- Karateke, A Kaplanoglu M, Avci F, et al. The Effect of Ramadan Fasting on Fetal Development.Pak. J Med Sci 31, 1295-1299 (2015).
- Rezk MAA, Sayyed T, AboElnasr M. et al. Impact of maternal fasting on fetal well-being parameters andfetal–neonatal outcome: A case-control study. J Matern Neonatal Med 29, 2834-2838 (2015).
- Altunkeser A, Körez MK. The Influence of Fasting in Summer on Amniotic Fluid DuringPregnancy. J Clin Imaging Sci 6, 21 (2016).
- 22. Mirghani H, Weerasinghe D, Ezimokhai M, et al. The effect of maternal fasting on the fetal biophysical profile. Int J Gynecol Obstet 81, 17-21 (2003).
- Seckin KD, Yeral MI, Karslı MF, et al. Effect of maternal fasting for religious beliefs on fetal sonographicfindingsand neonatal outcomes. Int J Gynecol Obstet 126 123-125 (2014).
- Boskabadi H Mehdizadeh A, Alboumiri Z. Effect of the Number of Ramadan Fasting Days on Maternal and NeonatalOutcomes. J Fasting Health 2, 84-89 (2014).
- Makvandi S, Nematy M, Karimi L. Effects of Ramadan Fasting on Neonatal Anthropometric Measurements in the Third Trimester of Pregnancy. Fast Health 1, 53-57 (2013).
- Sakar MN, Gultekin H, Demir B, et al. Ramadan fasting andpregnancy: Implications for fetal development in summer season. J Périnat Med 43, 319-323 (2015).
- 27. Alwasel S, Abotalib Z, Aljarallah J, et al. Changes in Placental Size during Ramadan. Placenta 31, 607-610 (2010).
- Jamilian H, Jamilian M, Hekmat PD, et al. The Effect of Ramadan Fasting on Outcome of Pregnancy. Middle-East J Sci Res 23, 1270-1275 (2015).
- Ozturk E, Balat O, Ugur MG, et al. Effect of Ramadan fasting on maternal oxidative stressduring the second trimester: A preliminary study. J Obstet Gynaecol Res 37, 729-733 (2011).
- Petherick ES, Tuffnell D, Wright J. Experiences and outcomes of maternal Ramadan fasting during pregnancy: Results from asub-cohort of the Born in Bradford birth cohort study. BMC Pregnancy Childbirth 14, 335 (2014).
- Safari K, Piro TJ, Ahmad HM. Perspectives and pregnancy outcomes of maternal Ramadan fasting in the second trimester of pregnancy. BMC Pregnancy Childbirth 19, 128 (2019).
- Sakar MN, Balsak D, Verit FF, et al. The effect of Ramadanfasting and maternal hypoalbuminaemia on neonatal anthropometric parameters and placental weight. J Obstet Gynaecol 36, 483-486 (2016).
- Sarafraz N, Abbaszadeh F, Bagheri A, et al. The Effect of Ramadan Fasting On Neonatal Weight In Different TrimestersOfPregnancy. Health Spiritual Med Ethics 2, 16-24 (2015).
- Savitri AI, Painter RC, Lindeboom M, et al. Ramadan exposure and birth outcomes: Apopulation-based study from the Netherlands. J Dev Orig Health Dis 11, 664-671 (2019).
[Google Scholar] [CrossRef]
- Tith RM, Bilodeau Bertrand M, Lee GE, et al. Fasting during Ramadan Increases Risk of Very PretermBirth among Arabic-Speaking Women. J Nutr 149, 1826-1832 (2019).
- Daley A, Pallan M, Clifford S, et al. Are babies conceived during Ramadanborn smaller and sooner than babies conceived at other times of the year? A Born in Bradford Cohort Study. J Epidemiol Community Health 71, 722-728 (2017).
- Savitri AI, Amelia D, Painter RC, et al. Ramadan during pregnancy and birth weight of newborns. J Nutr Sci 7, e5 (2018).
- Savitri AI, Yadegari N, Bakker J, et al. Ramadanfasting and newborn’s birth weight in pregnant Muslim women in The Netherlands. Br J Nutr 112, 1503-1509 (2014).
- Almond D, Mazumder B, Van Ewijk R. In UteroRamadan Exposure and Children’s Academic Performance. Econ J 125, 1501-1533 (2014).
- Sarafraz N, Atrian M, Abbaszadeh F, et al. Effect of Ramadan Fasting during Pregnancy on Neonatal Birth Weight. J Fasting Health 2, 37-40 (2014).
- Kavehmanesh Z, Abolghasemi H. Maternal Ramadan Fasting and Neonatal Health. J Perinatol 24, 748-750 (2004).
- Azizi F, Sadeghipour H, Siahkolah B, et al. Intellectual Development of Children Born of Mothers who Fasted in Ramadan during Pregnancy. Int J Vitam Nutr Res 74, 374-380 (2004).
- Majid MF. The persistent effects of in utero nutrition shocks over the life cycle: Evidence from Ramadan fasting. J Dev Econ 117, 48-57 (2015).
- Alwasel Sm, Abotalib Z, Aljarallah J, et al. Sex Differences in birth size and intergenerational effects of intrauterine exposure to Ramadan in Saudi Arabia. Am J Hum Biol 23, 651-654 (2011).
- Alwasel S, Harrath A, Aljarallah J, et al. Intergenerational effects of inutero exposure to Ramadan in Tunisia. Am J Hum Biol 25, 341-343 (2013).
- Pradella F, Van Ewijk R. As Long as the Breath Lasts: In Utero Exposure to Ramadan and the Occurrence of Wheezing in Adulthood. Am J Epidemiol 187, 2100-2108 (2018).
- Van Ewijk RJG, Painter RC, Roseboom TJ. Associations of Prenatal Exposure to Ramadan with Small Stature and Thinness in Adulthood: Results from a Large Indonesian Population-Based Study. Am J Epidemiol 177, 729-736 (2013).
- Nikoo MK, Shadman Z, Larijani B. Ramadan Fasting, Pregnancy and Lactation. Iran South Med J 17, 99-106 (2014).
- Arab M, Nasrollahi S. Interrelation of Ramadan Fasting and Birth Weight. Med J Islam World Acad Sci 14, 91-95 (2001).
- Awwad J, Usta I, Succar J, et al. The effect of maternal fasting during Ramadan on pretermdelivery: A prospective cohort study. BJOG Int J Obstet Gynaecol 119, 1379-1386 (2012).
- Cross JH, Eminson J, Wharton, BA. Ramadan and birth weight at full term in Asian Moslem pregnant women in Birmingham. Arch Dis Child 65, 1053-1056 (1990).
- Shahgheibi S, Ghadery E, Pauladi A, et al. Effects of Fasting during Third Trimester of Pregnancy onNeonatal Growth Indices. Ann Alquds Med 1, 58-62 (2005).
- Ziaee V, Kihanidoost Z, Yunesian M, et al. The Effect of Ramadan Fasting on Outcome of Pregnancy. Iran J Pediatr 20, 181-186 (2010).
- Moradi M. The effect of Ramadan fasting on fetal growth and Doppler indices of pregnancy. J Res Med Sci 16, 165-169 (2011).
- Karimi SM, Basu A. The effect of prenatal exposure to Ramadan on children’s height. Econ Hum Biol 30, 69-83 (2018).
- Kunto YS, Mandemakers JJ. The effects of prenatal exposure to Ramadan on stature during childhood and adolescence: Evidence from the Indonesian Family Life Survey Econ. Hum Biol 33, 29-39 (2018).
- Schoeps A, Van Ewijk R, Kynast Wolf G, et al. Ramadan Exposure In Utero and ChildMortality in Burkina Faso: Analysis of a Population-Based Cohort Including 41,025 Children. Am J Epidemiol 187, 2085-2092 (2018).
- Van Ewijk R. Long-term health effects on the next generation of Ramadan fasting during pregnancy. J Health Econ 30, 1246-1260 (2011).