Hybrid simulation for integrated skills teaching
- Corresponding Author:
- Katherine Joekes
St George’s, University of London Institute of Medical and Biomedical Education Cranmer Terrace, London E17 0RE, United Kingdom
Tel: +44 20 8725 0876
E-mail: kjoekes@sgul.ac.uk
Abstract
Background: Classroom teaching of communication and clinical skills in the pre-clinical years does not reflect authentic practice in the clinical workplace. This paper describes an innovative hybrid simulation teaching session on male urinary catheterisation to large cohorts of undergraduate medical students, which aims to achieve a holistic approach to integrated skills acquisition. Evaluation of the session is described.
Method: Undergraduate students (n=1221) took part in a 1-hour workshop, delivered over four years to consecutive cohorts. Evaluation forms (n=1042) captured students’ rating of the session and impact on their levels of confidence. Free text comments were explored using content analysis.
Results: The majority (91%) of students evaluated the sessions as excellent or good, with students who performed the procedure rating the session significantly higher. They did not feel more confident about their skills than students who merely observed. Free text comments illustrate perceived benefits of practising integration of clinical and communication skills.
Discussion: Teaching male catheterisation using hybrid simulation is effective, feasible and sustainable over time for large cohorts of undergraduate medical students. Students recognise benefits of learning communication and procedural skills in an integrated manner, and report increased levels of confidence in their ability to catheterise, provide explanations and build rapport with the patient
Keywords
Hybrid simulation; Male catheterization; Integrating communication and procedural skills; Undergraduate education
Introduction
An innovative ‘high fidelity’ simulation session was introduced to teach a large cohort of medical students an important clinical skill (i.e. male catheterisation) in a safe environment, whilst integrating essential communication and procedural skills. This paper reports on the rationale for this method, practical aspects of this teaching, and data from student evaluations. Classroom teaching of communication and clinical skills in the pre-clinical years does not reflect authentic practice in the clinical workplace, and may not transfer well to clinical practice [1], particularly when complex procedural skills are taught in isolation and while students lack experience. The use of ‘hybrid’ simulation [2], combining a manikin with a simulated patient, may contribute to solving this problem. Students can simultaneously practice complex practical skills (including “intimate” examinations) with explanation skills, while maintaining rapport through appropriate communication. This re-uniting of skills facilitates integration of knowledge, problem solving, clinical and communication skills in a more authentic environment. Simulation education [3], identifies the importance of learners being able to practice according to their own learning needs. This method has been used successfully in the teaching of clinical skills to undergraduate medical students, however, predominantly in the context of medium sized groups (25-50 learners) [4,5]. Skills may be retained and transferred to the clinical environment [6]. Simulation based teaching is recognized to contribute to improvement of patient safety [7]. The evaluation of the workshop explores whether: a) students found this integrated approach to skills teaching and learning worthwhile, and b) the session increases students’ levels of confidence. It did not assess competence.
Methods
▪ The teaching session
The aims: To teach a large cohort of undergraduate medical students the complex integrated clinical and communication skills of male urinary catheterisation.
The students: This session is scheduled in the “Transitional Year” (T-year), which bridges the gap between the classroom-based ‘clinical sciences’ phase of the course and the wardbased clinical years. Classroom-based blocks of learning alternate with clinical attachments.
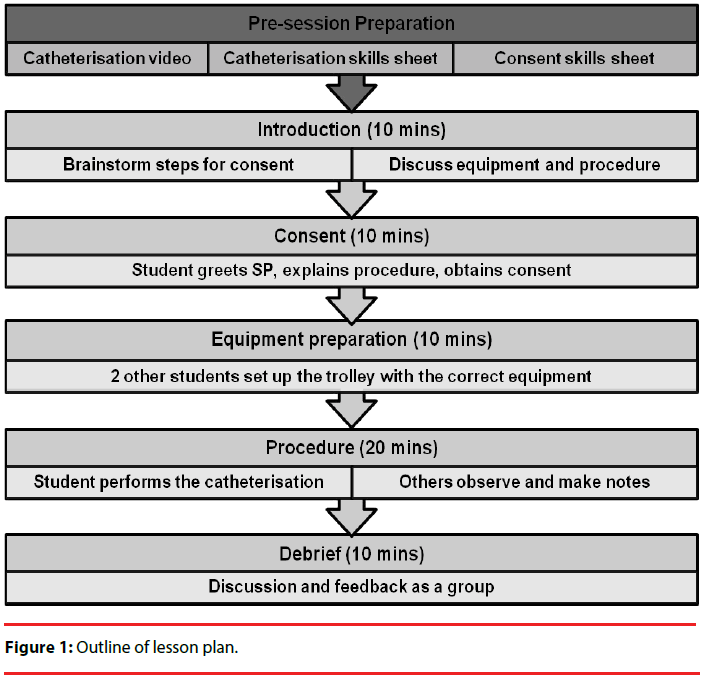
Session outline: Two filmed pilot sessions, with student volunteers, were observed and analysed by clinical and communication teaching faculty. The resulting teaching sessions were run as 1-hour workshops; i.e. 48 groups of 6-7 students per academic year. Students were instructed to prepare by revising notes from previous teaching [1], and to watch a skills video on male catheterisation. During the session all students actively identified i) steps for consent, ii) equipment needed and iii) steps of the catheterization procedure. Two students prepared equipment, one student performed the procedure, and one student documented the procedure in patient notes. The remaining students observed and offered feedback. A Communication Skills tutor and a Clinical Skills tutor worked collaboratively with each group of students, the latter acting as ‘clinical supervisor’ during the role play, while the former facilitated the process, monitored the Simulated Patient’s well-being (in role) and managed the feedback. A credible context for this high fidelity teaching was provided. The scenario portrays a patient with urinary retention post-surgery. Simulated Patients received a detailed briefing in order to standardize questions, mood and level of concern to be portrayed. During the catheterisation, the Clinical Skills tutor surreptitiously signaled to the SPs what level of discomfort/pain to portray, depending on the student’s performance. Students were unaware of this signaling.
▪ Student evaluation
Students completed an anonymous evaluation questionnaire after the teaching session, including questions regarding:
• Gender
• “How worthwhile was the workshop” (5-point Likert-type scale from ‘1=excellent’ to ‘5=very poor’)
• “As a result of the session, do you feel more confident in your ability to perform the technical aspects of the procedure” (5 point Likert-type scale from ‘1=very confident’ to ‘5=very unsure of myself’).
• “As a result of the session, do you feel more confident in your communication skills when catheterizing a patient” (5 point Likert-type scale from ‘1=very confident’ to ‘5=very unsure of myself’)
• “Any comments” (free text) to gather qualitative evaluation of the session
▪ Data analysis
Quantitative data analyses were carried out using IBM SPSS v19. Descriptive statistics were used. As the data was positively skewed and could not be corrected with transformations, non-parametric Mann-Whitney U tests were employed to compare the scores. Qualitative data were explored using Content Analysis as a flexible method for analysing text [8,9]. Two authors (KJ,LT) independently analysed the free text comments and formulated a set of themes, which were then discussed until full concordance on the meaning of each was achieved. These authors then independently coded the data set.
Results
Data were collected (n=1042) during four consecutive academic years (2009 – 2013). This represents 85% of the total number of students in these cohorts. Of the responders, 45% were male and 55% were female. This is representative of the group overall.
▪ Rating of the session
Students rated the session positively, with 50% rating the session as ‘excellent’, and 41% rating it as ‘good’. There was no difference in this rating between the four academic year groups. Students who performed the catheterisation task (n=164, Mdn=1 - excellent) rated the session significantly more positively than those students (n=841, Mdn=2 - good) who observed (Mann-Whitney U=42029, z=-8.84, p<0.001). There was no gender difference on how worthwhile the session was regarded.
▪ Self-rated confidence
Distribution (%) of self-reported confidence as a result of the session is reported in Table 1.
| Very Confident | Somewhat Confident | Neutral | Unsure of Self | Very Unsure of Self | |
|---|---|---|---|---|---|
| Confidence communicating with patient | 30.6 | 61.9 | 5.9 | 0.02 | 0 |
| Confidence performing the procedure | 19.6 | 64.9 | 11.8 | 1.6 | 0.3 |
Table 1: Percentage (%) of students self-rated confidence levels.
There was no significant difference in levels of self-reported confidence in communication or procedural skills, between the students who had performed the catheterisation during the session and those who had not (Mann- Whitney U=61938, z=-1.83, p=0.067, and Mann-Whitney U=65901, z=-0.27, p=0.791, respectively).
▪ Free text comments
Over the four years a total of 502 comments were given. These were categorised into 8 themes (see Table 2).
| Themes | % | Examples |
|---|---|---|
| Integration of skills | 23 | “It was really useful to integrate clinical & communication skills”; “Helpful to practice talking to the patient whilst doing the procedure” |
| Communication skills | 20 | “An excellent application of communication skills”; “I have learned a great deal in terms of consent, benefits and risks and how to convey this to the patient”. |
| Procedural skills | 17 | “Useful to have an opportunity to review/observe procedures as can be difficult to find opportunity on the wards.”; “Highlighted all the gaps in my knowledge of the procedure” ; “Good to practice” |
| Negative (general) | 17 | “Perhaps the session would be better at the start of the year” ; “Session too short” |
| Positive (general) | 9 | “Great session”; “Really really useful”; “Should have more sessions like these”. |
| Generic learning | 7 | “Good to go through consent and be patient-centred” ; “Good having multiple feedback” ; “I have realised I have a lot of work to do” |
| Too few opportunities | 5 | “Useful, but a session with opportunity for everyone to practice would have been even better” |
| Nerves & confidence | 2 | “Very reassuring”; Highlighted the importance of confidence” |
Table 1: Percentage (%) of students self-rated confidence levels.
Of note is that 11% of the comments (n=56) referred to the use of hybrid simulation, and specifically expressed how useful it had been to ‘splice’ the simulated patient with the catheter model (e.g. “Useful to have patients with model”; “…using an actor helped to make it feel more real”).
Discussion
The findings from the evaluation can be viewed in the light of both educational implications and practical considerations. Undergraduate medical students responded very positively to this integrated session and explicitly recognized the benefit of practicing this complex practical procedure, while also focusing on explanation skills and maintaining rapport with the patient. They report high levels of confidence, which echoes earlier findings [4]. Interestingly, students spontaneously generated comments about generic professional skills related to obtaining consent, showing respect and having a patientcentered approach, which they recognized as transferrable to other clinical situations. Due to time constraints and large cohort sizes, only one student per group performed the procedure, although three other students were actively involved and all students participated by providing guidance and feedback. This imbalance in tasks had from the outset raised concerns that students’ experience of this session would be inequitable. This was partly borne out by the fact that students who performed the catheterisation rated the session more positively, although evaluation scores show this difference to be small. In addition, several students identified this as a draw-back of the session. Importantly, there was no difference in the levels of confidence in skills acquisition between those students who performed the task versus those who observed, implying that all students gained equally in levels of confidence. From a practical perspective, this session is time-limited and deals with large cohorts, which was reflected in some negative comments made by the students (e.g. the timing within the curriculum, complicated logistics, and group sizes). In addition, these teaching sessions are labour-intensive and costly (approximately £10 per student, versus £5 if taught with single tutor and no SP). Regardless of these constraints, it has proved possible to sustain this teaching over subsequent years, allowing this innovative session to become part of the mainstream skills curriculum, and has led to the development of further integrated teaching (e.g. ‘Breast Examination and Explanation’).
Limitations
It is recognized that evaluation of this teaching is focused on student satisfaction and self-reported confidence, which is not an assessment of competence9. Therefore, conclusions about the impact of the teaching reported here on longterm competence and patient-safety cannot be drawn. Indeed a single one-hour teaching session could not be expected to have an effect at that level. The results of this evaluation, therefore, are viewed in the context of the broader curriculum, which places repeated emphasis on the necessity for students to develop their ability to integrate clinical skills, communication skills, knowledge and clinical reasoning.
Conclusion
The session shows that teaching male catheterisation in an integrated manner, using hybrid-simulation, is effective, feasible and sustainable for large cohorts of undergraduate medical students.
Declarations
The study was funded from the Institute’s own education budget. There is no conflict of interest that might bias the outcomes of the paper.
Acknowledgements
We are grateful to the participating students for completing the anonymous evaluation form. All students gave informed consent for the data to be used both internally (within our institution) and for publication.
Author Information
Katherine Joekes is a Chartered Health Pyschologist. She has a particular interest in the clinical communication skills which facilitate shared decision making and risk communication. Jo Brown is a Reader in Medical Education. She is passionate about education and is a National Teaching Fellow with an interest in clinical communication and academic support for students. Kerry Boardman is a General Practitionar and Senior Teaching Fellow involved in continuing professional development. She oversees quality of teaching in General Practice, with a particular interest in integrated consultation skills and clinical reasoning. She also provides academic support and is a student mentor and clinical adviser.
Laura Tincknel is currently an Intensive Care trainee, with a background in surgery and medical education.
Dason Evans is following a career in medical education and works clinically in sexual health.
Amy Spatz has a special interest in student and doctor well-being.
References
- Brown J (2012) Perspective: clinical communication education in the United Kingdom: some fresh insights. Acad Med 87: 1101-1104.
- Higham J, Nestel D, Lupton M, Kneebonen R (2007) Teaching and learning gynaecology examination with hybrid simulation. Clinical Teacher 4: 238-243.
- Kneebone R (2005) Evaluating clinical simulations for learning procedural skills: a theory-based approach. Acad Med 80: 549-553.
- Naylor AR, Hollett L, Valentine J, Mitchell I, Bowling M (2009) Can medical students achieve skills proficiency through simulated training? Amer J Surg 198: 277-282.
- Kneebone R, Kidd J, Nestel D, Asvall S, Paraskeva P (2002) An innovative model for teaching and learning clinical procedures. Medical Education 36: 628-634.
- Todson T, Henriksen M, Kromann C, Konge L, Eldrup J (2013) Short-and long-term transfer of urethral catheterization skills from simulation training to performance on patients. BMC Medical Education 13: 29.
- Aggarwal R, Mytton OT, Derbrew M, Hananel D, Heydenburg M (2010) Training and simulation for patient safety. QualSaf Health Care19: i34-i43.
- Hsieh H, Shannon S (2005) Three approaches to qualitative content analysis. Qual Health Res 15: 1277-1288.
- Kirkpatrick DL (1998) Evaluating Training Programmes. The four levels. (2nd Ed) San Fransisco; Berret-Koehler.