Intracardiac Echocardiography (ICE)-Guided External Iliac Transvenous Needle Biopsy of an Extravascular Retroperitoneal Mass
- Corresponding Author:
- Scott Resnick
Department of Radiology, Division of Interventional Radiology, Northwestern Memorial Hospital, Feinberg 4-710-x, Chicago, IL, 6061, U.S.A
E-mail: sresnick@northwestern.edu
Abstract
ABSTRACT
Although image-guided Percutaneous Needle Biopsy (PNB) is established as a safe procedure with a high technical success rate, biopsy target location and patient body habitus can limit procedure success. A 71-year-old with super-morbid obesity and two prior primary malignancies presented for biopsy of new retroperitoneal lymphadenopathy. Abdominal girth resulted in unsuccessful ultrasound and CTguided percutaneous biopsy attempts. An external iliac vein Transvascular Needle Biopsy (TVNB) was performed with a transjugular biopsy set under real-time intravascular ultrasound guidance using a wide-view Intracardiac Echo (ICE) probe. Specifically, midthigh left greater saphenous vein access was obtained for biopsy equipment as common femoral vein access was not obtainable due to body habitus. Biopsy samples were adequate for analysis. There were no vascular complications of vessel wall needle perforation or injury to adjacent structures.
Keywords
Biopsy; Obesity; Ultrasound; Clinical skills
Introduction
PNB is a routine procedure is considered lowrisk inexperienced hands using imaging guidance [1]. Technically successful procedures, defined by needle access to the target and a histologically adequate sample, are reported in the range of 71- 77% [2,3]. Non-operator dependent variables such as lesion size and location may contribute to technically unsuccessful procedures. Unsuccessful PNB delays treatment and diagnosis may require invasive surgical biopsy. In these situations, ICE-guided TVNB could provide an alternate approach for perivascular target lesions.
Materials and Methods
▪ Presentation
A 71-year-old man with super-morbid obesity and previously treated prostate and bladder cancers were referred to interventional radiology for biopsy of new left iliac lymphadenopathy. Histopathological diagnosis was necessary to differentiate between his two known primary malignancies and tailor systemic therapy. Attempted ultrasound and CT guided biopsies were both unsuccessful due to body habitus issues. Low-frequency trans-abdominal ultrasound (4MHz) had inadequate tissue penetration to image the target. CT-guided PNB with angled gantry required a >20 cm needle length to reach nodal targets in both supine and prone positions. This length, when added to the patient’s abdominal girth substantially exceeded the CT gantry diameter. Attempted transvascular biopsy of the pelvic nodal mass through the left external iliac vein using ICE guidance. Open surgical biopsy was discussed; however the patient was deemed a poor surgical candidate due to comorbidities
▪ Planning and materials
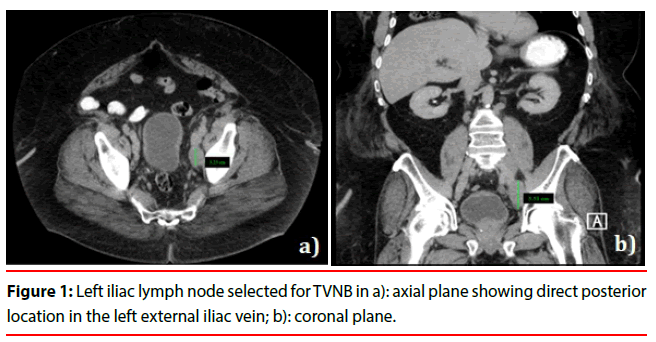
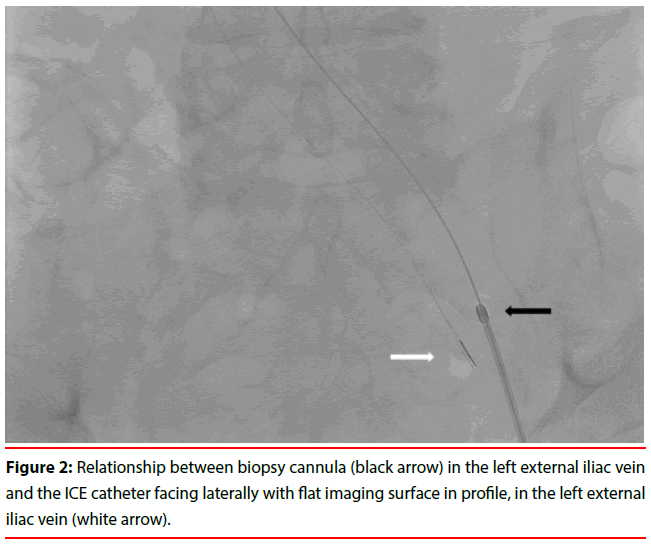
During planning, the authors identified the largest lymph node without an intervening structure, a 5.3 × 3.3 cm node posterior to the left external iliac vein (Figure 1). ICE (Siemens Acuson AcuNav catheter, Washington, DC) ultrasound was chosen as its lower frequency, typically 5-10MHz, and wide view provide optimal visualization of extraluminal structures relative to standard intravascular ultrasound (IVUS Phillips Volcano, Andover MA) which generally provides higher frequencies (10- 20MHz) for better intraluminal visualization. The authors planned a straight-line path (Figure 2) between the ICE probe right internal jugular vein (IJV) access site and biopsy needle guiding cannula in the left Common Femoral Vein (CFV) for the greatest maneuverability during the procedure. A biopsy would be performed with a standard Transjugular Liver Biopsy (TJLB) set.
Procedure Technique
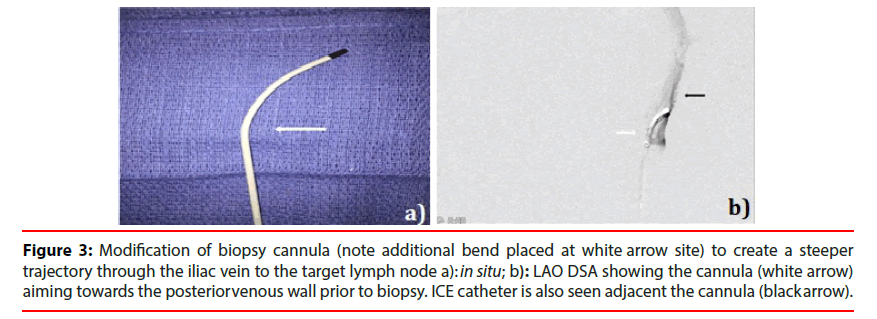
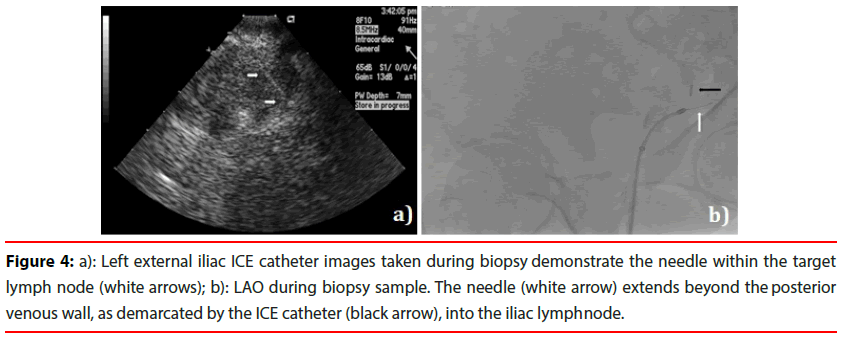
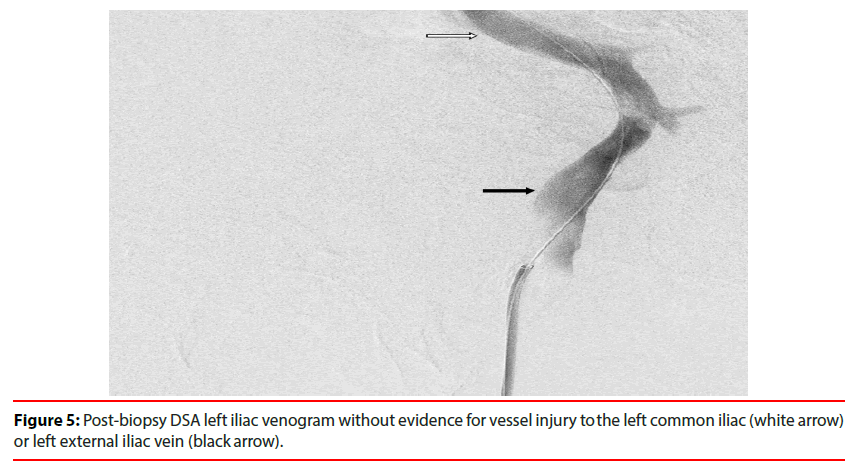
Informed consent was obtained. No IRB approval was required. The patient was positioned msupine. Body habitus prevented ready percutaneous access as the CFV depth was extreme and difficult to visualize as distinct from the adjacent artery. Using ultrasound guidance, right IJV and left midthigh GSV access were obtained and 9-French x 30 cm vascular sheaths were placed via each entry site. An ICE probe was advanced over a Glide Advantage guidewire (Terumo; Somerset, NJ) via the RIJ sheath and to the left external iliac vein near the expected level of the target node based on the pre-existing cross-sectional imaging information. The 19G transvenous liver biopsy guiding cannula (TLAB; Argon Medical Devices, Frisco TX) was advanced through the GSV sheath, over a Glide Advantage guidewire, and was positioned within the external iliac vein adjacent the ICE probe. The ICE catheter was used to identify the target node adjacent the external iliac vein. On fluoroscopy, the side-fire ICE probe has an asymmetric radiopaque line to indicate imaging direction such that when directed to the patient’s left, a 90-degree counterclockwise rotation will image posteriorly (Figure 2). The targeted lymph node was confirmed by size, abnormal ultrasound features, and expected location relative to the catheter direction and bony landmarks on fluoroscopy. The guiding cannula was modified by manually adding curvature to the distal end (Figure 3). This allowed the operators to direct the biopsy more posteriorly through the vascular wall over a relatively short distance. The biopsy needle was advanced towards the target using fluoroscopy and ICE guidance concurrently. The needle was visualized advancing into the lymph node sonographically before the sample was taken (Figure 4). Two core biopsies were evaluated by on-site touch prep cytology to confirm adequacy. Post-biopsy venogram through the GSV sheath did not demonstrate any contrast extravasation or evidence of vessel injury (Figure 5). After the instruments were removed, hemostasis was achieved with 5 minutes of manual compression.
Figure 3: Modification of biopsy cannula (note additional bend placed at white arrow site) to create a steeper trajectory through the iliac vein to the target lymph node a): in situ; b): LAO DSA showing the cannula (white arrow) aiming towards the posterior venous wall prior to biopsy. ICE catheter is also seen adjacent the cannula (black arrow).
Figure 4: Left external iliac ICE catheter images taken during biopsy demonstrate the needle within the target lymph node (white arrows); b): LAO during biopsy sample. The needle (white arrow) extends beyond the posterior venous wall, as demarcated by the ICE catheter (black arrow), into the iliac lymph node.
Results
The ICE-directed TVNB was technically successful. On-site touch prep cytology samples were deemed adequate by a board-certified cytopathologist and the presence of carcinoma was preliminarily confirmed. The final analysis revealed prostate adenocarcinoma, a surprising outcome since the expectation of the referring oncology service was for bladder cancer as the likely the culprit pathology. There were no immediate or delayed complications related to the access sites, vessel wall injury, or biopsy.
Discussion and Conclusion
As availability and operator experience with ICE and IVUS catheters increases, the utility of these devices has progressed from primarily diagnostic purposes to the enhancement of several vascular interventions. ICE-directed procedures first appeared in cardiac literature for atrial ablation and septal defect repair. Since case reports have described successful cardiac lesion biopsy using a combination of fluoroscopy and ICE-guidance for real-time visualization [4,5]. More recent studies in interventional radiology have demonstrated that ICE can decrease complication rates and procedure times when used during transjugular intrahepatic portosystemic shunt creation [6,7]. In order to perform TVNB, the operators selected an 8MHz ICE transducer to identify and target retroperitoneal lymphadenopathy that exceeded the tissue penetration depth of a standard transabdominal transducer.
The selection between ICE and IVUS for procedure guidance depends on the depth needed to image the lesion. High-frequency IVUS transducers image depths up to 2-5 cm with high resolution in 360-degrees. This capability makes it useful for interventions requiring a close assessment of the vessel wall and lumen such as during stent deployment, iliocaval reconstruction, and May-Thurner intervention [8,9]. Conversely, ICE transducers are typically lower in frequency, providing a greater imaging depth and 90-degree imaging. The trend of successful ICE and IVUS-guided procedures suggests that there are indeed more uses for these instruments.
A transvenous biopsy was performed with a curved TJLB set. The operators modified the set by manually bending a steeper distal curve to more directly transgress the venous wall. The steeper curve allowed the needle trajectory to pass over relatively short distances such that the needle and target could be visualized with ICE throughout the biopsy.
Parameters for safe venous transgression in a non-compressible location were considered prior to biopsy. In a hemodynamically stable adult, the thoracoabdominal cavity acts as a hydraulic system and maintains a balanced pressure gradient promoting a venous return to the heart. Resting intraabdominal pressures range from 9.5 ± 5 mmHg supine to 16.9 ± 7.2 mmHg erect and have even higher baseline levels in morbidly obese patients [10,11]. Given the normal central venous pressures of 3-8 mmHg, the pressure gradient should theoretically promote intravascular blood flow and hemostasis after venipuncture. However, even in the context of abdominal pressure being greater than intravascular pressure, bleeding complications may still arise. In addition, factors such as plasma protein volume, platelet count, and coagulopathy contribute to the tendency for hemorrhage and were appropriately assessed before transvenous biopsy. Patients who meet standard coagulation minimums (INR>1.5, platelets>50,000, without antiplatelet or anticoagulation medications) should have a reasonable expectation of hemostasis after the procedure.
Indeed, the literature supports select cases of venous transgression without significant complications. Transcaval liver biopsy has been performed in patients with inaccessible hepatic veins such as in Budd-Chiari [12]. Sofocleous et al describe CT-guided biopsy of pancreatic and peripancreatic lesions by traversing the inferior vena cava or renal vein for 18-22 G fine needle aspiration [13]. Finally, transcaval procedures such as CT-guided transcaval radiofrequency ablation with an 18G electrode and transcaval TAVR in patients with small iliofemoral vessels or advanced atherosclerosis have also been described [14,15]. In the case of retroperitoneal TVNB, the operators performed a post-biopsy venogram to assess for vascular injuries, such as extravasation and were prepared to treat endovascularly should any of those complications arise.
Although the procedure is limited by its singular nature, conclusions may still be drawn from this and similar reports. First, ICE or IVUS can provide real-time biopsy guidance for perivascular lesions not visible with transabdominal ultrasound. Selection between ICE and IVUS should be made based upon the size and proximity of a lesion to the catheterized vein. Operator experience and comfort level with intravascular ultrasound may contribute to procedural success. Second, although iliofemoral and caval transgression should not be a primary technique, there is evidence to suggest it can be performed safely for biopsy of lymph nodes that are in complicated locations and/or in patients whose body habitus limit the efficacy of standard image-guided methods. Evaluation of the patient’s coagulation parameters, comorbidities, and medications is crucial to identify patients in whom transvenous biopsy may pose a greater bleeding risk. Post-biopsy venogram should be performed to identify immediate complications and the appropriate tools should be immediately available to treat if necessary. Finally, as ICE and IVUS become more commonly used in interventional radiology procedures, additional studies will be necessary to determine the impact on procedural success, overall complication rates, and procedure time.
References
- Gupta S, Wallace MJ, Cardella JF, et al. Quality improvement guidelines for percutaneous needle biopsy. J Vasc Interv Radiol 21(7), 969-975 (2010).
- Zhao J, Li L, Peng L. Safe and effective guidance by intracardiac echocardiography for transcatheter closure in atrial septal defects. Int J Clin Exp Med 8(6), 9815-9819 (2015).
- Daoud EG, Kalbfleisch SJ, Hummel JD. Intracardiac echocardiography to guide transseptal left heart catheterization for radiofrequency catheter ablation. J Cardiovasc Electrophysiol Mar 10(3), 358-363 (1999).
- Takashima A, Ogata T, Yamada H, et al. Intracardiac echocardiography guided biopsy of a lipomatous cardiac tumor arising from the interatrial septum. Circ J 81(10), 1553-1555 (2017).
- Higo T, Takemoto M, Ogawa K, et al. Intracardiacm, Echocardiography-guided cardiac tumor biopsy. Circulation 73, 381-383 (2009).
- Pillai AK, Andring B, Faulconer N, et al. Utility of intravascular US-guided portal vein access during transjugular intrahepatic portosystemic shunt creation: Retrospective comparison with conventional technique in 109 patients. J Vasc Interv Radiol 27(8), 1154-1159 (2016).
- Gipson MG, Smith MT, Durham JD, et al. Intravascular US-guided portal vein access: Improved procedural metrics during tips creation. J Vasc Interv Radiol 27(8), 1140-1147 (2016).
- Marrocco CJ, Jaber R, White RA, et al. Intravascular ultrasound. Semin Vasc Surg 25(3), 144-152 (2012).
- Majdalany BS, Khaja MS, Williams DM. Intravascular ultrasound-guided intervention for may-thurner syndrome. Semin Intervent Radiol 34(2), 201-207 (2017).
- Al-Hwiesh A, Al-Mueilo S, Saeed I, et al. Intraperitoneal pressure and intra-abdominal pressure: Are they the same? Perit Dial Int 31(3), 315-319 (2011).
- De Keulenaer B, De Waele J, Powell B, et al. What is normal intra-abdominal pressure and how is it affected by positioning, body mass and positive end-expiratory pressure? Intensive Care Med 35(6), 969-976 (2009).
- Mammen T, Keshava SN, Eapen CE, et al. Transjugular liver biopsy: A retrospective analysis of 601 cases. J Vasc Interv Radiol 19(3), 351-358 (2008)
- Sofocleous CT, Schubert J, Brown KT, et al. CT-guided transvenous or transcaval needle biopsy of pancreatic and peripancreatic lesions. J Vasc Interv Radiol 15(10), 1099-1104 (2004).
- Akhlaghpoor S, Dahi F, Alinaghizadeh M, et al. CT fluoroscopy-guided transcaval radiofrequency ablation of insulinoma. J Vasc Interv Radiol 22(3), 409-410 (2011).
- Shaikh S, Song T, Wang DD, et al. Transcaval TAVR-what the radiologist needs to know. Current Cardiovascular Imaging Reports 8(9), 1-8 (2015).