Obstructive Sleep Apnea Risk Assessment among Type 2 Diabetes and its Relation to Neck Circumference
- Corresponding Author:
- Khaled Alswat
Dean of Graduate Studies
Consultant Physician of Internal Medicine
Diabetes and Endocrinology
Certified Clinical Densitometrist
Taif University School of Medicine
Taif, Saudi Arabia
E-mail: kalswat@hotmail.com
Abstract
Background
Type 2 Diabetes Mellitus (T2D) is a chronic illness that is wide spreading worldwide. Obstructive Sleep Apnea (OSA) is clinically defined as a group of disorders diagnosed by recurrent apneas. Our primary goal is to assess the prevalence of high risk OSA in a random sample of T2D patients.
Method
This is a cross-sectional descriptive study conducted between November 2015 and July 2016. We interviewed adult T2D patients who had routine follow-up visits. Patients with type I and gestational diabetes mellitus, untreated hypothyroidism, and those with goiter were excluded. We used STOP-Bang Questionnaire to assess OSA risk.
Result
A total of 216 patients were participated in the study with a mean age of 60.9+11.1 years, predominantly male and with long standing T2D. 54.2% of the patients have a low/intermediate risk for OSA. Compared to those who were considered to have low/intermediate risk, those who have high risk were older (p=0.171), and mostly male (p<0.001), have longer duration of T2D (p=0.002), higher BMI (<0.001), higher waist circumference (<0.001 ), neck circumference (<0.001), higher SBP (p=0.324), higher HbA1c (p=0.706), physically inactive (p=0.312), and were more likely to have cardiac disease (p=0.002 ) and retinopathy (p=0.009).
There was a significant positive correlation between the neck circumference and OSA risk score (r=0.229, p=0.001).
Conclusion
45.8% of our patients have a high risk for OSA. Those were more likely to be older male, have longer T2D duration, higher measures of adiposity, worse cardiovascular markers, poor lifestyle habits, and were more likely to have complications.
Keywords
Obstructive sleep apnea; OSA; Diabetes mellitus; T2D; STOP-bang questionnaire; Neck circumference
Introduction
Type 2 diabetes mellitus (T2D) is a chronic illness that is wide-spreading worldwide. 415 million adult people have diabetes according to The International Diabetes Federation’s (IDF) in 2015 and this number will rise to 642 million in less than 25 years [1]. The prevalence of diabetes in Saudi Arabia showed a higher progression over the past three decades. The recent cross-sectional study included more than 20000 participants, recorded that 34.5% was the overall prevalence of abnormal glucose metabolism with 22.6% of them having prediabetes and 11.9% having diabetes [1].
Obstructive Sleep Apnea Syndrome (OSAS) is clinically defined as a group of disorders diagnosed by recurrent apneas (complete cessation of breathing) and/or hypopneas (shallow breathing) during sleep. Obstructive sleep apnea (OSA) is by far the most common sleep disorders in the general population [2]. This condition is predicted to affect approximately 2%-4% of the general population with a prevalence that even much higher based on demographic variables such as age, sex, and BMI [3]. A cross-sectional study of obese men and premenopausal women sleeping less than 6.5 hours per night found OSAS in 58% and concluded that increased neck circumference (NC) is associated with OSAS and metabolic syndrome in obese men and premenopausal women [4]. Turkish study showed that NC of >39 cm for men and NC of >35 for women represent the optimal cutoff that accurately predicted OSA [3].
The clinical symptoms of OSA are extensive and include sleepiness during daytime, decrease in quality of life, and raised susceptibility toward driving-related accidents [5-8]. Kinds of literature theorize that sleep apnea is associated with fasting hyperglycemia, insulin resistance, and T2D [9]. Other studies showed that snoring women are at increased risk for cardiovascular disease, T2D and metabolic syndrome [10]. An observational cohort study that examined 1233 patients concluded that OSA is a risk factor for type 2 diabetes [11].
The American College of Physicians recommends polysomnography as the diagnostic test in patients with suspected of OSA [12]. A recent study suggested that 40% of patients with OSA will have T2D [13]. While other studies showed that 23% of T2D patients have OSA [14]. To screen for OSA several questioners exist, one of the most popular one is Berlin Questioner and most recently validated is the STOP-Bang questioner. The sensitivity of STOP-Bang score ≥ 3 to detect moderate to severe and severe OSA is 93% and 100% respectively [15]. IDF recently published a consensus that recommends OSA screening for T2D patients particularly those with classical OSA symptoms with the two-stage approach in which a structured questionnaire used first followed by formal sleep study for those who considered being high-risk patients [16].
At our center we are lacked for a sleep lab and sleep specialist. Our primary goal in this study is to screen a random sample of T2D patients for OSA using STOP-Bang Questioner to identify the prevalence of high-risk OSA. Also to identify the clinical characteristics of high-risk patients for OSA compared to those considered low risk for OSA.
Methods
A cross-sectional descriptive study carried out on T2D patients attending the Prince Mansour Military Hospital, Diabetes Center, Taif, Saudi Arabia from the beginning of November 2015 to the end of July 2016. Type I diabetes mellitus and Gestational diabetes mellitus patients, untreated hypothyroidism, and those with goiter were excluded. The participation was voluntary and verbal consent was taken from each participant. The study protocol runs in compliance with the IRB regulations at the Military Hospital where our proposal was reviewed and approved. Our sample size was 216 patients. All subjects were T2D patients attending the prince Mansour Military Hospital, Diabetes Center Taif, Saudi Arabia. After reassuring the guardians about the confidentiality of the study and the information it contains, an informed verbal consent obtained from all of them. Data was collected through an interview and self-report questionnaire at the time of regular patients visits.
Researchers interviewed patients and collected personal data, methods of management, DM complications, and social habits and completed the STOP-Bang questioner. Anthropometric measures were taken as well as blood pressure and Body Mass Index (BMI) was calculated. Recent lab work data were collected from files using the subjects’ medical record numbers. We considered those who reported monthly income > 4000 US dollars as high income while those reported monthly income <1335 US dollars as low income. A number of severing hypoglycemic episodes in the past 12 months were self-reported.
We used STOP-Bang Questionnaire to assess for the OSA risk with score range 0-8. Patients were asked to recall if they experienced any snoring, tiredness, observed by anyone chocked or stopped their breathing during sleep, hypertension, BMI more than 35 kg/m2, age older than 50, neck size measured around Adams apple in males (17 inches/43 cm) or larger and in females (16 inches/41 cm) or larger and male gender as a risk. we considered OSA-Low risk if the yes questions were 0-2 questions, intermediate-risk if the yes questions were 3-4 questions and high risk if the yes questions were 5-8 questions or if yes to 2 or more of 4 STOP questions plus male gender or if yes to 2 or more of 4 STOP questions plus BMI >35 kg/m2 or if yes to 2 or more of 4 STOP questions plus neck circumference 17 inches/43 cm in male or 16 inches/41 cm in female.
Data were coded, entered and analyzed using SPSS software program version 20 for analysis. According to the type of data, the following tests were used to test differences for significance; Chi-square for qualitative variables and t-test for quantitative variables. Correlations between variables were carried out. Mean and standard deviation were calculated for quantitative data. The results were presented in the appropriate forms of tables and graphs.
Results
A total of 216 patients participated in the study with a mean age of 60.9 years (SD 11.1), predominantly male with long-standing T2D with mean HbA1c 8.9 (SD 2.1) and the mean BMI of 32.2 (SD 5.8) kg/m2 (Table 1). Most of the patients were married and have low income but minorities with Bachelor’s degrees or higher.
| Baseline characteristics (N= 216) | |
|---|---|
| Mean age (yrs) | 60.9+11.1 |
| Male (%) | 53.7 |
| Mean diabetes duration (years) | 14.5+8.4 |
| Mean BMI (Kg/m2) | 32.3+5.8 |
| Mean waist circumference (cm) | 109.8+12.5 |
| Mean neck circumference (cm) | 40.3+4.4 |
| Mean systolic blood pressure (mmHg) | 131.8+20.0 |
| Mean diastolic blood pressure (mmHg) | 73.1+9.6 |
| Socioeconomic | |
| Married (%) | 93.5 |
| Bachelor degree or higher (%) | 4.6 |
| Low income (%) | 61.6 |
| High income (%) | 2.3 |
| Complications | |
| Hypoglycemia (%) | 29.2 |
| Retinopathy (%) | 44.9 |
| Neuropathy (%) | 56.5 |
| Renal failure (%) | 3.7 |
| Cardiac disease (%) | 18.5 |
| Medications | |
| Diet (%) | 0.9 |
| Oral hypoglycemic agents (%) | 33.3 |
| Insulin (%) | 9.3 |
| Oral hypoglycemic agents and insulin (%) | 56.5 |
| ACE inhibitors (%) | 51.4 |
| Statin (%) | 78.7 |
| Laboratory data | |
| Fasting glucose (mmol/L) | 9.9+4.2 |
| HbA1c (%) | 8.9+2.1 |
| Total cholesterol (mmol/L) | 4.5+0.9 |
| LDL (mmol/L) | 2.6+0.8 |
| HDL (mmol/L) | 1.0+0.3 |
| Triglyceride (mmol/L) | 1.7+1.0 |
| ACR | 26.2+103.6 |
| Calculated GFR (ml/min/1.73 m2) | 80.5+20.8 |
| Lifestyle habits | |
| Sedentary lifestyle (%) | 58.3 |
| Exercise > 150 min / week | 21.3 |
| Active smoking (%) | 8.3 |
Table 1: Baseline characteristics of the whole cohort.
The most common T2D complications were neuropathy followed by retinopathy. The management of T2D in our participants were varies, with more than half of them were on oral hypoglycemic agents together with insulin and 1/3 were on oral hypoglycemic agents only. Most patients were on statin and ACE inhibitors.
Majorities of patients reported a sedentary lifestyle and only 21.3% of the patient’s exercise >150 minutes per week. Few patients were active smokers.
54.2% of the patients have a low/intermediate risk for OSA according to the STOP-Bang score. Compared to those who were considered to have low/intermediate risk, those who have high risk were older (p=0.171), and mostly male (p<0.001), have longer duration of T2D (p=0.002), higher BMI (<0.001), higher waist circumference (<0.001), neck circumference (<0.001), higher SBP (p=0.324), higher HbA1c (p=0.706), physically inactive (p=0.312), and were more likely to have cardiac disease (p=0.002 ) and retinopathy (p=0.009 ). Although those who were high risk for OSA were more likely to be on oral hypoglycemic agents plus insulin and on a statin, both groups tend to have comparable lipid control.
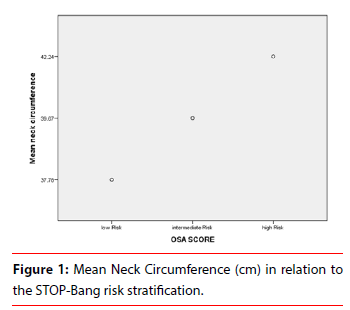
There was a positive correlation between the neck circumference and OSA risk score (Figure 1). Partial correlation between NC and OSA risk adjusting for age, gender, duration of T2D, marital status, income, educational level, and BMI showed a significant positive correlation (r=0.229, p=0.001) (Table 2).
| Low/Intermediate risk | High risk | p-value | |
|---|---|---|---|
| Baseline characteristic | |||
| Number of patients | 117 | 99 | n/a |
| Mean age (yrs) | 60.0+11.4 | 62.0+10.7 | 0.171 |
| Male (%) | 40.2 | 69.7 | <0.001 |
| Mean diabetes duration (years) | 12.9+7.8 | 16.3+8.7 | 0.002 |
| Mean BMI (Kg/m2) | 30.9+5.1 | 34.1+6.1 | <0.001 |
| Mean waist circumference (cm) | 105.2+9.9 | 115.2+13.1 | <0.001 |
| Mean neck circumference (cm) | 38.7+4 | 42.2+4 | <0.001 |
| Mean systolic blood pressure (mmHg) | 130.5+19.4 | 133.2+20.7 | 0.324 |
| Mean diastolic blood pressure (mmHg) | 73.4+9.8 | 72.7+9.5 | 0.549 |
| Socioeconomic | |||
| Married (%) | 92.3 | 95 | 0.3 |
| Bachelor degree or higher (%) | 4.3 | 5.1 | 0.551 |
| Low income (%) | 60.7 | 62.6 | 0.937 |
| High income (%) | 2.6 | 2 | |
| Complications | |||
| Hypoglycemia (%) | 25.6 | 33.3 | 0.215 |
| Retinopathy (%) | 36.8 | 54.6 | 0.009 |
| Neuropathy (%) | 50.4 | 63.6 | 0.051 |
| Renal failure (%) | 2.6 | 5.1 | 0.335 |
| Cardiac disease (%) | 11.1 | 27.3 | 0.002 |
| Medications | |||
| Diet (%) | 1.7 | 0 | 0.086 |
| Oral hypoglycemic agents (%) | 39.3 | 26.3 | |
| Insulin (%) | 9.4 | 9.1 | |
| Oral hypoglycemic agents and insulin (%) | 49.6 | 64.6 | |
| ACE inhibitors (%) | 41.9 | 62.6 | 0.002 |
| Statin (%) | 72.6 | 85.9 | 0.018 |
| Laboratory data | |||
| Fasting glucose (mmol/L) | 9.6+4 | 10.3+4.4 | 0.244 |
| HbA1c (%) | 8.81+2.2 | 8.91+1.8 | 0.706 |
| Total cholesterol (mmol/L) | 4.5+0.9 | 4.5+0.9 | 0.903 |
| LDL (mmol/L) | 2.6+0.7 | 2.6+0.8 | 0.987 |
| HDL (mmol/L) | 1.1+0.3 | 1.0+0.2 | 0.143 |
| Triglyceride (mmol/L) | 1.8+1.1 | 1.7+0.9 | 0.728 |
| ACR | 29.7+131.7 | 22.3+56.3 | 0.62 |
| Calculated GFR (ml/min/1.73 m2) | 82.8+19.6 | 77.9+21.9 | 0.088 |
| Lifestyle habits | |||
| Sedentary lifestyle (%) | 54.7 | 62.6 | 0.312 |
| Exercise > 150 min / week | 25.6 | 16.2 | |
| Active smoking (%) | 6.8 | 10.1 | 0.387 |
Table 2: Baseline characteristics based on STOP-Bang score.
Discussion
In our study, the prevalence of a low/intermediate risk for OSA according to the STOP-Bang score was 54.2% of the patients while those who have high risk were 45.8% and mostly male. In contrast to this other studies which showed that the prevalence of mild OSA (defined by Apnea- Hypopnea Index (AHI) ≥ 5) were ranging from 3% to 28%; and for moderate OSA (defined by AHI ≥ 15) were ranging from 1 to 14% and those were predominantly white men and women with mean BMI of 25 kg/m-28 kg/m [3]. With the different screening tool, we used for OSA screening its difficult to frame our results in context with the former mentioned findings.
Our findings showed that patients with high-risk OSA had higher fasting glucose and HbA1c and were more likely to be on oral hypoglycemic agents plus insulin. Also, those with highrisk OSA in our study were more likely to be physically inactive and to have cardiac diseases and retinopathy. In cohort studies reported that OSA is significantly related to lower general health status and increases the risk of developing T2D and impaired glucose tolerance [7,11,13] Other Population-based studies indicate that habitual snoring is independently associated with glucose intolerance and insulin resistance [9]. Our data showed most of the high-risk OSA patient on a statin, Previous studies agreed with our result as they reported the significant effect of OSA on lipid metabolism and profile which associated with cardiovascular diseases and cognitive performance [17,18].
Our study showed a significant positive correlation between the NC and OSA risk scores after adjusting for possible confounders. A retrospective study showed that larger NC was associated with OSAS and in obese men and premenopausal women [19]. NC is significantly larger in those with severe OSAS independent of the other possible risk factors for severe OSAS [19-23].
Our strengths included using a standardized new validated tool (the STOP-Bang score), comprehensive medical history and laboratory data. Our limitations included a single center and a small sample size.
Conclusion
The majority of our patients have a low/ intermediate risk for OSA according to the STOP-Bang score. Compared to those who were considered to have low/intermediate risk, those who have high risk were mainly older, male, have a longer duration of T2D, higher BMI, higher waist circumference, neck circumference, higher SBP, higher HbA1c, physically inactive, and were more likely to have complications. There was a positive correlation between the neck circumference and OSA risk score.
Conflict of Interest
None
References
- Al-Nozha MM, Al-Maatouq MA, Al-Mazrou YY, et al. Diabetes mellitus in saudi Arabia. Saudi Med J 25, 1603-1610 (2004).
- Punjabi NM and Polotsky VY. Disorders of glucose metabolism in sleep apnea. J Applied Physiol 99, 1998-2007 (2005).
- Young T, P.E. Peppard, and D.J. Gottlieb, Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 165, 1217-1239 (2002).
- Cizza G, de Jonge L, Piaggi P, et al. Neck circumference is a predictor of metabolic syndrome and obstructive sleep apnea in short-sleeping obese men and women. Metab Syndr Relat Disord 12, 231-241 (2014).
- Daniel JG, Coralyn WW, William HB, et al. Relation of sleepiness to respiratory disturbance index: the Sleep Heart Health Study. Amer J Res Crit Care Med 159, 502-507 (1999).
- Baldwin CM, Grifith KA, Nieto J, et al. The association of sleep-disordered breathing and sleep symptoms with quality of life in the sleep heart health study. Sleep 24, 96-105 (2001).
- Finn L, Young T, Palta M, et al. Sleep-disordered breathing and self-reported general health status in the wisconsin sleep cohort study. Sleep 21, 701-708 (1998).
- George CF. Sleep· 5: Driving and automobile crashes in patients with obstructive sleep apnoea/hypopnoea syndrome. Thorax 59, 804-807 (2004).
- Punjabi NM, Shahar E, Redline S, et al. Sleep-disordered breathing, glucose intolerance, and insulin resistance. Am J Epidemiol 136, 167-178 (2003).
- Leineweber C, Kecklund G, Akerstedt T, et al. Snoring and the metabolic syndrome in women. Sleep Med 4, 531-536 (2003).
- Botros N, Concato J, Mohsenin V, et al. Obstructive sleep apnea as a risk factor for type 2 diabetes. Am J Med 122, 1122-1127 (2009).
- Qaseem A, Dallas P, Owens DK, et al. Diagnosis of obstructive sleep apnea in adults: A clinical practice guideline from the american college of physicians diagnosis of obstructive sleep apnea in adults. Ann Intern Med 161, 210-220 (2014).
- Meslier N, Gagnadoux F, Giraud P, et al. Impaired glucose-insulin metabolism in males with obstructive sleep apnoea syndrome. Eur Respir J 22, 156-160 (2003).
- West SD, Nicoll DJ, Stradling JR, et al. Prevalence of obstructive sleep apnoea in men with type 2 diabetes. Thorax 61, 945-950 (2006).
- Chung F, Abdullah HR, Liao P, et al. STOP-Bang questionnaire: A practical approach to screen for obstructive sleep apnea. Chest 149, 631-638 (2016).
- Paul J, George S. IDF Consensus of screening Diabetics for obstructive sleep apnea. International Diabetes Feeration. (2008).
- Lavie L, Vishnevsky A, Lavie P. Evidence for lipid peroxidation in obstructive sleep apnea. Sleep 27, 123-128 (2004).
- Peng Y, Zhou L, Cao Y, et al. Relation between serum leptin levels, lipid profiles and neurocognitive deficits in Chinese OSAHS patients. Int J Neurosci 127, 981-987 (2017).
- Cizza G, de Jonge L, Piaggi P, et al. Neck circumference is a predictor of metabolic syndrome and obstructive sleep apnea in short-sleeping obese men and women. Metab Syndr Relat Disord 12, 231-241 (2014).
- Ahbab S, AtaoÃâßlu HE, Tuna M, et al. Neck circumference, metabolic syndrome and obstructive sleep apnea syndrome; evaluation of possible linkage. Med Sci Monit 19, 111-117 (2013).
- Lim YH, Choi J, Kim KR, et al. Sex-specific characteristics of anthropometry in patients with obstructive sleep apnea: neck circumference and waist–hip ratio. Ann Otol Rhinol Laryngol 123, 517-523 (2014).
- Davies R, Ali NJ, Stradling JR. Neck circumference and other clinical features in the diagnosis of the obstructive sleep apnoea syndrome. Thorax 47, 101-105 (1992).
- Onat A, Hergenç G, Yüksel H, et al. Neck circumference as a measure of central obesity: Associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference. Clin nut 28, 46-51 (2009).