Tooth autotransplantation : A systematic review of the literature
- Corresponding Author:
- Maroua Garma,Department of oral medicine and oral surgery, Laboratory of oral health and maxillofacial rehabilitation, University clinic of Dental Medicine, University of Monastir, Tunisia (LR12ES11)
E-mail: marwa.garma@yahoo.fr
Received: 12-Dec 2023, Manuscript No. IJOCS-24-122602; Editor assigned: 14-Jan-2024, PreQC No. IJOCS-24-122602(PQ); Reviewed: 10-Feb-2024, QC No. IJOCS-24-122602(Q); Revised: 20- Feb-2024, Manuscript No. IJOCS-24- 122602(R); Published: 15-Mar2024, DOI: 10.37532/1753- 0431.2024.18(1).240
Abstract
Introduction: Tooth auto transplantation is a proposed alternative to missing teeth replacement. Various cases of this technique are reported, Consequently, many benefits, limits and outcomes of tooth auto transplantation are discussed in the literature. The aim of this study was to perform a systematic review of the literature to highlight advantages and disadvantages of this option, it’s outcomes and different influencing factors.
Materials and Methods: A Medline search was conducted via PubMed from 2010 to March 2022. Mesh key words were used and combined with different Boolean operator.
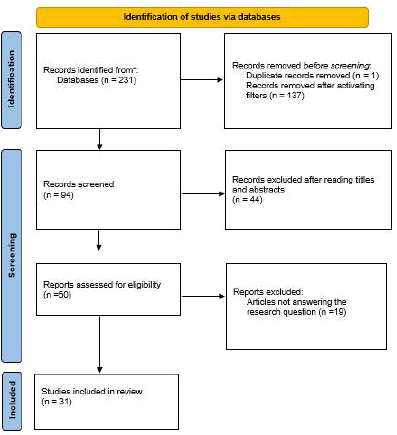
Results: The electronic search led to 231 articles. After activating filters, duplicates removal and respecting inclusion and exclusion criteria, 31 articles were selected for the review.
Discussion: According to this review, tooth auto transplantation is a well-documented technique. Various influencing factors were reported and discussed. It was approved by the majority of authors due to its benefits and the hight level of its controlled outcomes.
Keywords
Auto transplantation; Tooth; Prognosis; Success; Outcomes
Introduction
Patients may often exhibit early loss of teeth resulting from congenital reasons, traumatic dental injury, caries. Consequently, vacated space filling is mandatory. Various treatment alternatives are proposed such as: implant supported restoration, removal partial denture, fixed bridges, orthodontic space closure and auto transplantation.
Since that, many cases of tooth auto transplantation were performed and published. As a result, this treatment option is very well documented in the literature.
In fact, according to the different publication, auto transplantation has many benefits. Its success is related to many criteria: clinical and radiological finding, presence of ankylosis, root resorption, mobility, periodontal healing and survival rate.
This success and the prognosis of this act is influenced by many preoperative, peroperative and postoperative factors.
The aim of this study was to conduct a systematic review of literature in order to highlight different outcomes of auto transplantation and to assess the effect of various influencing factors.
Clinical relevance
Tooth autotransplantation is the transplantation of a tooth from its original site into a receiving site. It is a well-documented alternative for the replacement of missing teeth. A variety of outcomes were reported as well as a variety procedure. That’s motivate this review, which aimed to evaluate different outcomes of this alternative to better decide the therapeutic choice and to precisely know the different protocols, especially that a new one was describe: cone beam guided surgical procedure.
According to this review, average of controlled outcomes was in favor of tooth auto transplantation. The different surgical procedure described have sufficient results.
Literature Review
■Materials and methods
An electronic search was performed on Medline via “PubMed”. The following filters were activated: date: from 2010 to March 2022 and species: humans.
The Mesh keywords used were: Tooth”, “Transplantation, Autologous”, “Survival rate”, “Prognosis”, “Tooth Mobility”, “Tooth Ankylosis”, “Root Resorption”, “Dental Pulp Diseases”.
The Mesh terms were combined in the search field as follow:
The search algorithm was:
“Tooth” AND “Transplantation, Autologous” AND (“Survival rate” OR “Prognosis” OR “Tooth Mobility” OR “Tooth Ankylosis” OR “Root Resorption” OR “Dental Pulp Diseases” OR “Success rate”).
Inclusion criteria: Controlled trials and prospective/retrospective studies;
• Studies reporting at least one of the following outcomes: success rate, survival rate, mobility, presence of ankylosis, root resorption and pulp condition of auto transplanted teeth.
Exclusion criteria: Editorials, letters, grey literature, traditional reviews, systematic reviews, meta-analysis, perspective, and letter to the editor and comparative studies case reports and case series;
• Articles not treating the subject of tooth autologous transplantation.
• Articles not answering the research question.
• Studies reporting primary auto transplanted teeth.
• Articles published in a language other than French or English.
Data directly related to measures of the outcomes of interest were recorded and extracted. The outcomes evaluated were as follows: success rate, survival rate, degree of mobility, pulp conditions, root resorption and ankylosis of the auto transplanted teeth.
Data extracted from eligible articles after full text screening process included study details (author, year of publication, study type and its aim), the number of participants and their demographics (age and gender), details about the auto transplantation procedure (number and group of donor teeth and the recipient site, root development stage, Mean follow-up duration, conventional or guided surgery) and finally the outcomes.
Results
The Medline search via PubMed database identified a total of 231 articles. After screening by activating filters, duplicates removal and respecting inclusion and exclusion criteria, only 31 articles were selected for the review. The result of bibliographic research is detailed in (Figure 1).
Among the 31 included articles, 27 were retrospective [3-29].
Three were prospective studies [30-32]. One of them was controlled clinical trial [33].
The sample size of the included studies ranged from 17 to 552 patients, with a mean sample of 83 patients. The majority of studies assessed auto transplantation in young patients, with a mean age of 20 years.
The most commonly transplanted teeth reported in selected studies were premolars, third molars and then canines. Both mature and immature teeth were transplanted and for those with incomplete root formation, the developmental root stage were mostly reported at stage 4 or 5 at the time of the surgery.
The indications of tooth auto transplantation described in the included articles were: agenesis, trauma, tooth loss due to pathological processes such as periodontal disease or tooth decay and endodontic or restorative hopeless prognosis.
The follow-up period varied among the studies from 0 year to 29 years, with a mean period of 6 years.
Characteristics of the outcome measures
Reported outcomes of auto transplantation included: survival rate, success rate, degree of mobility, pulp condition, root resorption and ankylosis.
For the survival rate: 15 articles described a survival rate after 1 year ranging from 75.3% to 100% with a mean of 91.98%.
A survival rate after 5 years was reported in 9 articles ranging between 78% to 100% with an average of 89.3%. Ten articles reported a survival rate after 10 years with a mean of 78.68% and ranging from 59.1% to 95%. After 15 years, the survival rate was reported in 3 articles: 54.5%, 85% and 28% and in one article, it was 81.5% for a follow up period up to 20 years.
For the success rate, 15 articles reported a success after 1 year with a mean of 75.12% and ranging from 32% to 93%. After 5 years, the success rate was described in 7 articles with an average of 68.42% and range between 31% and 86%. The success rate after 10 years was reported in 4 articles with a mean of 66.8%. After 20 years, the success rate was reported in one article and it was 67.9%.
For the degree of mobility, it was the less assessed outcome. Only 10 of the included studies have reported the degree of mobility of auto transplanted teeth postoperatively with a mean rate of 5.35% of the total number of auto transplanted teeth and ranging from 0% to 12.71%.
For the outcome concerning pulp condition, root canal treatment was performed in all cases with closed apices. For this outcome, we have focused mainly on the results of revascularization of auto transplanted immature teeth. Almost all authors of the included articles agreed that pulp obliteration appears to be an early, normal and potential physiologic sign of pulp healing and it was seen in all auto transplanted immature teeth. Their pulp healing was examined in 11 articles and they reported a mean rate of 56.81% and a range from 30% to 100%.
The inflammatory root resorption after auto transplantation was observed and reported in 22 included articles with a mean rate of 15.38% and a range from 0% to 51%.
The last outcome which was ankylosis or replacement resorption was assessed also in 22 articles and showed a mean rate of 14.18% with a range from 0% to 42%.
Discussion
The terminology of auto transplantation was first introduced by Fleming and Hoek et al. and is slightly modified by Joseph R et al [34]. It’s defined as the transplantation of tooth from one site to another in the same individual.
For the tooth auto transplantation procedures, both the conventional surgical procedure and the cone beam guided one are reported with a comparable efficiency and sufficient results.
According to the literature, there is no standardized success criteria of auto transplantation but the majority of studies reported the same outcomes that should be controlled to judge the success of this act such as survival rate, success rate, degree of mobility, pulp condition, root resorption and ankylosis.
Most of included articles agreed this technique and all results particularly the high average of controlled outcomes was in favor this option.
According to different selected articles, numerous risk factors were arguably approved to influence the results of tooth auto transplantation. These influencing factors were classified in three categories: subject-related factors, procedural factors and postoperative factors.
For the subject-related factors, age is the first influencing factor as auto transplantation presents usually favorable results with patients under 20 years old and may confront some difficulties or failure for patients aged more than 45 years [35,36]. The second factor is gender, this technique showed a higher success rate in females [37]. Tooth auto transplantation seems to have better prognosis when it concerns canine, premolar or incisor compared to multirooted teeth. This may be due to the root anatomy of anterior teeth and the easiest surgical access that facilitate the transplantation procedure, besides to the fact that posterior teeth have higher masticatory forces to support interfering consequently the healing and the stabilization of transplanted tooth [23].
Concerning the factor of root development stage, the majority of authors recommended transplanting teeth having the stage 4 or 5 of Moorrees [38].
The viability of periodontal ligament cells is one of the important factors for the successful adaptation of the donor tooth to recipient site, as a result erupted teeth show favorable outcomes than partially or not erupted teeth [39].
The recipient site should have adequate thickness of the buccal and lingual cortical bone and should have a good quality with no infection or previous ankylosis of the extracted tooth to not influence negatively the success of the transplant.
Several studies in the review reported some procedural factors influencing the success of tooth auto transplantation. In fact, favorable outcomes require easy and atraumatic surgical intervention with an experienced operator [5,40- 42].
The majority of authors recommended to minimize the extra-alveolar time of the donor tooth as much as possible and to preserve it in an appropriate storage such as saline or Hank’s balanced Salt solution [8,13].
For the tooth stabilization after transplantation, sutures seem to be sufficient and more appropriate than composite-wire splinting and for the two methods, stabilization shouldn’t exceed 14 days [43,44].
It is preferable to perform a root canal treatment for mature teeth after transplantation and to promote revascularization of immature teeth to obtain better results of this technique [45,46].
Finally, for the category of postoperative factors, the first influencing factor is the immediate loading of auto transplanted tooth, for it finding of the review suggest avoiding occlusal forces during the first week of healing [47,48].
The second one is the postoperative orthodontic treatment which when associated to tooth auto transplantation after one week contribute to a better prognosis.
The strong point of this review (the favor) is the fact that it includes various articles of various types: retrospective, prospective and control clinical trial. These articles focused in the different outcomes of tooth auto transplantation with a long term follow up and in the different factors influencing the prognosis.
Nevertheless, this review presents some limits. The important one is that most of included studies are retrospective and prospective and only one controlled clinical trial, this classifies the review as having a lower level of evidence. The inexistence of a consensus of the surgical protocol and defined specific criteria determining the success of tooth auto transplantation in the literature besides to the variability of average of controlled outcomes in the different articles lead to the creation of heterogeneity in this study.
Conclusion
Tooth auto transplantation is an alternative option to the replacement of missed teeth that has been widely documented in the literature and its effectiveness was discussed by many authors. According to the current performed review, although the different limitations revealed, we can conclude that this therapeutic option can be a successful method that should be recommended. Nevertheless, additional studies of high level of evidence are required such as observational studies of a larger samples and randomized controlled trial to conclude a standardized consensus of successful criteria and surgical procedure of this option.
References
- Machado, L. A., Do Nascimento, R. R., et al. Long-term prognosis of tooth autotransplantation: a systematic review and meta-analysis. J Oral Maxillofac Surg. 45(5), 610-617 (2016). [Google Scholar] [CrossRef]
- Atala-Acevedo, C., Abarca, J., Martínez-Zapata, et al. Success rate of autotransplantation of teeth with an open apex: systematic review and meta-analysis. J Oral Maxillofac Surg. 75(1), 35-50 (2017). [Google Scholar] [CrossRef]
- de Freitas Coutinho, N. B., Nunes, F. C., et al. Success, survival rate, and soft tissue esthetic of tooth autotransplantation. J Endod. 47(3), 391-396 (2021). [Google Scholar] [CrossRef]
- Kafourou , V., Tong, H. J., Day, P., et al. Outcomes and prognostic factors that influence the success of tooth autotransplantation in children and adolescents. Dent Traumatol. 33(5), 393-399 (2017). [Google Scholar]
- Juslin, J., Jääsaari, P., Teerijoki-Oksa, T., et al. Survival of Autotransplanted teeth with open apices: A retrospective cohort study. J Oral Maxillofac Surg. 78(6), 902-e1(2020). [Google Scholar] [CrossRef]
- Lucas‐Taulé, E., Llaquet, M., Muñoz‐Peñalver, J., et al. Mid‐term outcomes and periodontal prognostic factors of autotransplanted third molars: A retrospective cohort study. J Periodontol. 92(12), 1776-1787 (2021). [Google Scholar] [CrossRef]
- Boschini, L., Melillo, M., & Berton, F. Long term survival of mature autotransplanted teeth: A retrospective single center analysis. J Dent. 98, 103371. (2020) [Google Scholar] [CrossRef]
- Grisar, K., Nys, M., The, V., Vrielinck, L., et al. Long‐term outcome of autogenously transplanted maxillary canines. Clin Exp Dent Res. 5(1), 67 (2020) [Google Scholar] [CrossRef]
- Wu, Y., Chen, J., Xie, F., et al. Autotransplantation of mature impacted tooth to a fresh molar socket using a 3D replica and guided bone regeneration: two years retrospective case series. BMC Oral Health. 19, 1-8 (2019). [Google Scholar] [CrossRef]
- Patel, S., Fanshawe, T., Bister, D., et al. Survival and success of maxillary canine autotransplantation: a retrospective investigation. Eur J Orthod. 33(3), 298-304 (2011). [Google Scholar] [CrossRef]
- Gonnissen, H., Politis, C., Schepers, S., et al. Long-term success and survival rates of autogenously transplanted canines. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontology. 110(5), 570-578 (2010). [Google Scholar] [CrossRef]
- Yoshino, K., Ishizuka, Y., Sugihara, N., et al. Gender difference in tooth autotransplantation with complete root formation: a retrospective survey. J Oral Rehabil. 40(5), 368-374 (2013). [Google Scholar] [CrossRef]
- Mertens, B., Boukari, A., & Tenenbaum, H. Long‐term follow up of post‐surgical tooth autotransplantation: a retrospective study. J Investig Clin Dent. 7(2), 207-214 (2016). [Google Scholar] [CrossRef]
- Kvint, S., Lindsten, R., Magnusson, A., et al. Autotransplantation of teeth in 215 patients: a follow-up study. Angle Orthod. 80(3), 446-451 (2010). [Google Scholar] [CrossRef]
- Yoshino, K., Kariya, N., Namura, D., et al. Survival rate in autotransplanted premolars with complete root formation: a retrospective clinical survey. Bull Tokyo Dent Coll. 54(1), 27-35 (2013). [Google Scholar] [CrossRef]
- Huth, K. C., Nazet, M., Paschos, E.,et al. Auto transplantation and surgical uprighting of impacted or retained teeth: a retrospective clinical study and evaluation of patient satisfaction. Acta Odontol Scand.1538-1546 (2013). [Google Scholar] [CrossRef]
- Verweij, J. P., Toxopeus, E. E., Fiocco, M., et al. Success and survival of autotransplanted premolars and molars during short‐term clinical follow‐up. J Clin Periodontol. 43(2), 167-172 (2016). [Google Scholar] [CrossRef]
- Abela, S., Murtadha, L., Bister, D., et al. Survival probability of dental autotransplantation of 366 teeth over 34 years within a hospital setting in the United Kingdom. . Eur J Orthod. 41(5), 551-556 (2019). [Google Scholar] [CrossRef]
- Abella, F., Ribas, F., Roig, M., et al. Outcome of autotransplantation of mature third molars using 3-dimensional–printed guiding templates and donor tooth replicas. J Endod. 44(10), 1567-1574 (2018). [Google Scholar] [CrossRef]
- Stange, K. M., Lindsten, R., et al. Autotransplantation of premolars to the maxillary incisor region: a long-term follow-up of 12–22 years. Eur J Orthod. 38(5), 508-515 (2016). [Google Scholar] [CrossRef]
- Watarai, H., Warita, H., & Soma, K.. Effect of nitric oxide on the recovery of the hypofunctional periodontal ligament. J Dent Res. 3(4), 338-342 (2004). [Google Scholar] [CrossRef]
- Vilhjálmsson, V. H., Knudsen, G. C., Grung, B., et al. Dental auto‐transplantation to anterior maxillary sites. Dent Traumatol. 27(1), 23-29 (2011). [Google Scholar] [CrossRef]
- Tang, H., Shen, Z., Hou, M., et al. Autotransplantation of mature and immature third molars in 23 Chinese patients: a clinical and radiological follow-up study. BMC Oral Health. 17(1), 1-9 (2017). [Google Scholar] [CrossRef]
- Jang, Y., Choi, Y. J., Lee, S. J., et al. Prognostic factors for clinical outcomes in autotransplantation of teeth with complete root formation: survival analysis for up to 12 years. J endod. 42(2), 198-205 (2016). [Google Scholar] [CrossRef]
- Aoyama, S., Yoshizawa, M., Niimi, K., et al. Prognostic factors for autotransplantation of teeth with complete root formation. Oral Surg Oral Med Oral Pathol Oral Radiol. 114(5), S216-S228 (2012). [Google Scholar] [CrossRef]
- Denys, D., Shahbazian, M., Jacobs, R., et al. Importance of root development in auto transplantations: a retrospective study of 137 teeth with a follow-up period varying from 1 week to 14 years. Eur J Orthod. 35(5), 680-688 (2013). [Google Scholar] [CrossRef]
- Yoshino, K., Kariya, N., Namura, D., et al. A retrospective survey of auto transplantation of teeth in dental clinicsJ. oral rehabil. 39(1), 37-43 (2012). [Google Scholar] [CrossRef]
- Raabe, C., Bornstein, M. M., Ducommun, J., et al. A retrospective analysis of autotransplanted teeth including an evaluation of a novel surgical technique. Clin oral investig. 25, 3513-3525 (2021). [Google Scholar] [CrossRef]
- Shahbazian, M., Jacobs, R., Wyatt, J., et al. Validation of the cone beam computed tomography–based stereolithographic surgical guide aiding autotransplantation of teeth: clinical case–control study. Oral Surg Oral Med Oral Pathol Oral Radiol. 115(5), 667-675 (2013). [Google Scholar] [CrossRef]
- de Carvalho, V. M., de Carvalho, C. M., de Carvalho, et al. Statistical analysis of teeth auto transplantation in Portugal's region of Chaves. Acta Odontol Scand. 72(3), 179-186 (2014). [Google Scholar] [CrossRef]
- Nagori, S. A., Bhutia, O., Roychoudhury, A., et al. Immediate autotransplantation of third molars: an experience of 57 cases. Oral Surg Oral Med Oral Pathol Oral Radiol. 400-407 (2014). [Google Scholar] [CrossRef]
- Plakwicz, P., Wojtowicz, A., & Czochrowska, E. M. Survival and success rates of autotransplanted premolars: a prospective study of the protocol for developing teeth. Am J Orthod Dentofac Orthop. 144(2), 229-237 (2013). [Google Scholar] [CrossRef]
- Grisar, K., Smeets, M., Ezeldeen, M., et al. Survival and success of autotransplanted impacted maxillary canines during short‐term follow‐up: A prospective case‐control study. Orthodontics & Craniofacial Research, 24(2), 222-232. (2021). [Google Scholar] [CrossRef]
- Natiella, J. R., Armitage, J. E., & Greene, G. W. The replantation and transplantation of teeth: A review. Oral Surg Oral Med Oral Pathol Oral Radiol. 29(3), 397-419 (1970). [Google Scholar] [CrossRef]
- Kingsmill, V. J. Post-extraction remodeling of the adult mandible. Crit Rev Oral Biol Med. 10(3), 384-404 (1999). [Google Scholar] [CrossRef]
- Michl, I., Nolte, D., Tschammler, C., et al. Premolar autotransplantation in juvenile dentition: quantitative assessment of vertical bone and soft tissue growth. Oral Surg Oral Med Oral Pathol Oral Radiol. 124(1), e1-e12 (2017) [Google Scholar] [CrossRef]
- Shiau, H. J., & Reynolds, M. A. Sex differences in destructive periodontal disease: a systematic review. J Periodontol. 81(10), 1379-1389 (2010). [Google Scholar] [CrossRef]
- Moorrees, C. F., Fanning, E. A., & Hunt Jr, E. E. Age variation of formation stages for ten permanent teeth. J Dent Res. 42(6), 1490-1502 (1963). [Google Scholar] [CrossRef]
- Gilijamse, M., Baart, J. A., Wolff, J., et al. Tooth auto transplantation in the anterior maxilla and mandible: retrospective results in young patients. Oral Sur Oral Med Oral Pathol Oral Radiol. 122(6), e187-e192 (2016). [Google Scholar] [CrossRef]
- Andreasen, J. O., & Kristerson, L. The effect of limited drying or removal of the periodontal ligament: periodontal healing after replantation of mature permanent incisors in monkeys. Acta Odontol Scand. 39(1), 1-13 (1981). [Google Scholar] [CrossRef]
- Andreasen, J. O., Paulsen, H. U., Yu, Z., et al. A long-term study of 370 autotransplanted premolars. Part III. Periodontal healing subsequent to transplantation. Eur J Orthod. 12(1), 25-37 (1990). [Google Scholar] [CrossRef]
- Jonsson, T., & Sigurdsson, T. J. Autotransplantation of premolars to premolar sites. A long-term follow-up study of 40 consecutive patients. Am J Orthod Dentofac Orthop. 125(6), 668-675 (2004). [Google Scholar] [CrossRef]
- Tsukiboshi, M. Autotransplantation of teeth: requirements for predictable success. Dent Traumatol. 18(4), 157-180 (2002). [Google Scholar] [CrossRef]
- Lundberg, T., & Isaksson, S. A clinical follow-up study of 278 autotransplanted teeth. Br J Oral Maxillofac Surg. 34(2), 181-185 (1996). [Google Scholar] [CrossRef]
- Coolidge, E. D. The thickness of the human periodontal membrane. J Am Dent Assoc Dent Cosm. 24(8), 1260-1270 (1937). [Google Scholar] [CrossRef]
- Tsukiboshi, M., Yamauchi, N., & Tsukiboshi, Y. Long-term outcomes of autotransplantation of teeth: a case series. J endod. 45(12), S72-S83 (2019). [Google Scholar] [CrossRef]
- Mine, K., Kanno, Z., Muramoto, T., et al. Occlusal forces promote periodontal healing of transplanted teeth and prevent dentoalveolar ankylosis: an experimental study in rats. Angle Orthod. 75(4), 637-644 (2005). [Google Scholar] [CrossRef]
- Nayak, B. N., Wiltshire, W. A., Ganss, B., et al. Healing of periodontal tissues following transplantation of cells in a rat orthodontic tooth movement model. Angle Orthod. 78(5), 826-831(2008). [Google Scholar] [CrossRef]